Hürthle Cell Carcinoma: Staging and Treatment
What is staging for cancer?
Staging is the process of learning how much cancer is in your body and where it is. Tests like ultrasound, thyroid uptake and scan (using radioactive iodine), CT, MRI, and PET scan may be done to help stage your cancer. Your providers need to know about your cancer and your health so that they can plan the best treatment for you.
Staging looks at the size of the tumor and where it is, and if it has spread to other organs. The staging system for thyroid cancer is called the “TNM system,” as described by the American Joint Committee on Cancer. It has three parts:
- T-describes the size/location/extent of the "primary" tumor in the thyroid.
- N-describes if the cancer has spread to the lymph nodes.
- M-describes if the cancer has spread to other organs (called metastases).
Your healthcare provider will use the results of the tests you had to determine your TNM result and combine these to get a stage from 0 to IV.
How is Hürthle cell carcinoma staged?
Hürthle cell carcinoma is staged as a thyroid cancer. Staging is based on:
- The size of your tumor on imaging tests and what is found after surgery.
- Any evidence of spread to other organs (metastasis).
- Surgery to test if your lymph nodes have cancer cells.
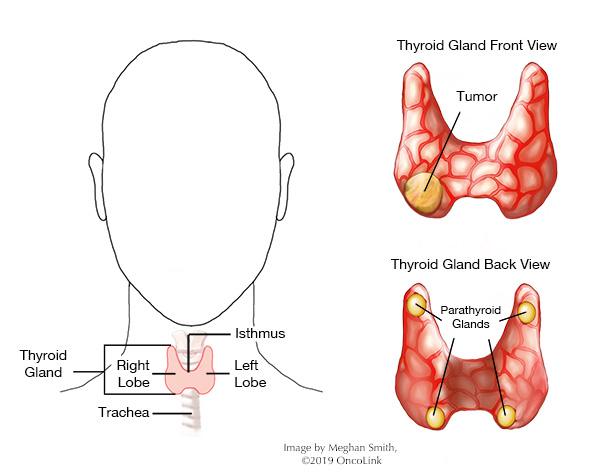
Staging for thyroid cancer also looks at the size of your tumor, your age, and if you have major capsular invasion. Major capsular invasion means the tumor is close to the thyroid junction (gaps where cells pass through), and the tumor has grown into the fat and tissue around the thyroid.
The staging system is very complex. Below is a summary of the staging system. Talk to your provider about the stage of your cancer.
- Stage I:
- Younger than 55 years old and the cancer is any size, and it might or might not spread to nearby lymph nodes. It has not spread to distant sites.
- You are 55 years or older and the cancer is no bigger than 2 cm across and is found only in the thyroid. It has not spread to lymph nodes or distant sites.
- You are 55 years or older, the cancer is between 2 cm and 4 cm across and only in the thyroid. It has not spread to the lymph nodes or distant sites.
- Stage II:
- Younger than 55 years old, the tumor is any size, may or may not spread to nearby lymph nodes, and has spread to other parts of the body like distant lymph nodes, other organs, or bones.
- You are 55 years or older and the cancer is no larger than 2cm across and only in the thyroid, but, it has spread to nearby lymph nodes.
- You are 55 years or older and the cancer is between 2 cm and 4 cm across, confined to the thyroid, and has spread to nearby lymph nodes.
- You are 55 years or older and the cancer is larger than 4cm, confined to the thyroid, or has grown into the strap muscles around the thyroid. It may or may not spread to nearby lymph nodes.
- Stage III:
- You are 55 years or older and the cancer is any size and has grown into nearby tissues of the neck like the larynx, trachea, esophagus, or the nerve to the larynx. It may or may not have spread to nearby lymph nodes.
- Stage IV:
- IVA: You are 55 years or older and the cancer is any size, it has grown beyond the thyroid back towards the spine or large blood vessels. It may or may not have spread to nearby lymph nodes.
- IVB: You are 55 years or older and the cancer is any size, may or may not have spread to nearby lymph nodes but has spread to other parts of the body.
How is Hürthle cell carcinoma treated?
Treatment for Hürthle cell carcinoma is based on your cancer stage, age, overall health, and testing results. Your treatment may include some or all of the following:
- Surgery.
- Radioactive Iodine.
- Radiation Therapy.
- Clinical Trials.
Surgery
The main treatment used is surgery. Some tumors will grow faster than others and that will guide what type of surgery you have. The size of the cancer, your age, and your health will also help decide which surgery you will have. In some cases, the whole thyroid gland is removed (total thyroidectomy) along with any enlarged lymph nodes. If cancer is found in any lymph nodes you may need a lymph node dissection. In other cases, only part of the thyroid will be removed.
Radioactive Iodine
Radioactive iodine is given into a vein (IV, intravenously) and the thyroid cells take in this iodine. The radioactive iodine delivers radiation to these cells killing them. It may be used after surgery to kill any normal thyroid tissue left behind after surgery. It is often used to treat thyroid cancer and some cases of Hürthle cell cancer.
Radiation Therapy
Radiation is the use of high-energy x-rays to kill cancer cells. In Hürthle cell carcinoma, radiation therapy is used to treat symptoms of metastases (like pain and nausea), to control recurrent tumors (tumors that have come back), and to prevent recurrence (stopping the tumor from coming back). It may also be used if the whole thyroid is not removed during surgery.
Clinical Trials
You may be offered a clinical trial as part of your treatment plan. To find out more about current clinical trials, visit the OncoLink Clinical Trials Matching Service.
Making Treatment Decisions
Your care team will make sure you are included in choosing your treatment plan. This can be overwhelming as you may be given a few options to choose from. It feels like an emergency, but you can take a few weeks to meet with different providers and think about your options and what is best for you. This is a personal decision. Friends and family can help you talk through the options and the pros and cons of each, but they cannot make the decision for you. You need to be comfortable with your decision – this will help you move on to the next steps. If you ever have any questions or concerns, be sure to call your team.
You can learn more about thyroid cancer at OncoLink.org.
References
American Cancer Society. Thyroid Cancer.
Aytug S et al. Hurthle Cell Carcinoma. Medscape. 2023. Found at: http://emedicine.medscape.com/article/279462
Goffreddo P et al. Hurthle Cell Carcinoma. Cancer. 2012. 119(3):504-511.
Munari-Silem Y. (1996). Gap Junctions in the Thyroid Gland: Distribution, Regulation, Function. National Library of Medicine. https://pubmed.ncbi.nlm.nih.gov/9084695/
PDQ Cancer Information Summaries. Thyroid Cancer Treatment. 2024. Found at: http://www.ncbi.nlm.nih.gov/books/NBK65719/
Zheyu Yang, Jian Zhou, Lei Tao, & Wei Cai. (2023). Central and lateral neck involvement in papillary thyroid carcinoma patients with or without thyroid capsular invasion: A multi-center analysis. Frontiers in Endocrinology, 14. https://doi.org/10.3389/fendo.2023.1138085