Total Body Irradiation (TBI)
Total Body Irradiation (TBI) is when your whole body (front and back/head to toe?) gets radiation therapy. The radiation given is a low dose so that normal tissues can repair (heal) themselves. TBI is used in several types of cancer, such as leukemias, lymphomas, multiple myeloma, and some solid tumors.
TBI may be given for any of the following reasons:
- To kill the cancer cells in the areas where surgery, local (focused) radiation and chemotherapy can’t easily get to, like your nervous system, bones, skin, or testes.
- As part of a bone marrow or stem cell transplant so that your immune system does not reject the transplanted cells. Radiation lowers the response of your immune system so that your body doesn’t see the transplanted cells as foreign and rejects them.
- To make room for new bone marrow to grow and make healthy blood cells (engraftment) after your transplant.
How is a treatment plan created?
You will have a CT scan of your body. In some cases, measurements of certain areas of your body will be done, instead of a CT scan, to create your treatment plan.
How is TBI given?
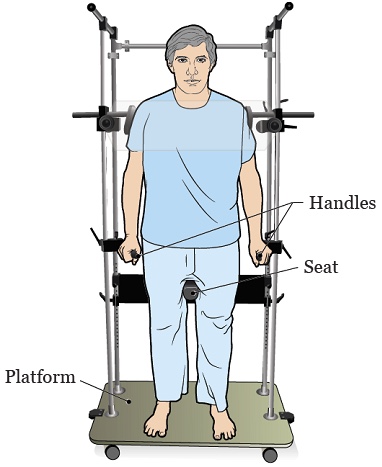
You will either stand or lie down during the treatment. The following devices are used to keep you in position:
- TBI stand or platform.
- Treatment couch.
- Table or stretcher.
You will be far away from the treatment machine where the radiation comes from. The radiation is usually given to the front of your body first. Then the radiation therapist will help you turn 180 degrees so that they can deliver the rest of the radiation to your back.
What is the treatment schedule?
TBI is usually given over 1-5 days. You will get two to three treatments a day 4 to 6 hours apart. This treatment schedule is important to reach our goal of destroying your bone marrow and/or suppressing your immune system prior to having your bone marrow or stem cell transplant.
The bone marrow or stem cells to be transplanted are given back to you through an IV (intravenous) following the last radiation treatment. The transplant team and the radiation therapy team will work together to coordinate the delivery of your radiation treatment and stem cell or bone marrow transplant.
What treatment devices are used?
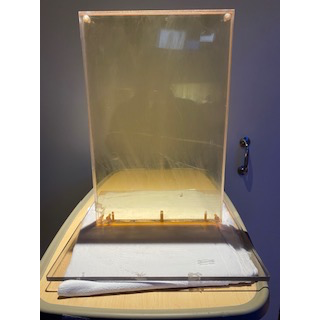
Head and Neck Compensators
Head and neck compensators are thick lead devices that are placed on a plastic tray. The head and neck compensator will be placed in front of your head and neck for treatment if the radiation team decides it is needed. These are used to even out the treatment dose for differences in size between your head and neck.
TLD - Thermoluminescent dosimeters
On the first day of treatment, small circular measuring devices called TLDs will be placed on your skin by one of the members of the radiation physics team. They are placed on your skin to make sure the radiation dose is equally given to the front and back of your body. The devices are taped on your skin for treatment in the following areas:
- Ankles.
- Knees.
- Thighs.
- Back.
- Head.
- Neck.
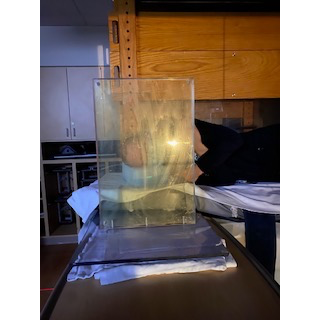
Lung and Renal Blocks
Lung and renal (kidney) shielding (blocks) are sometimes used during treatment. Lungs and kidneys are sensitive to radiation so your provider may use them to lower the amount of radiation they get. These blocks are usually made of lead or alloy. They are made specifically for you and match the shape of your lungs and kidneys.
What if I have concerns during treatment?
You will see the radiation therapist every day for treatment and can ask them questions or report any concerns. Your radiation oncologist will see you 1- or 2-times during treatment, depending on your treatment schedule. Report any concerns about side effects to your care team.
What are the possible acute side effects of TBI?
Acute side effects are those that you have right away or soon after treatment. Side effects can vary from person to person. Make sure to talk to your care team about any new or concerning side effects you have.
- Nausea and Vomiting: Nausea and vomiting can be a common side effect. You may be given medications to help manage this side effect. Eat foods that you feel you can tolerate and try to get enough fluids so that you stay hydrated.
- Diarrhea: The radiation may cause diarrhea since radiation is being given to the whole body. It is important to stay hydrated. You may be given medications to help manage this side effect.
- Mucositis (Mouth sores): These sores can make it hard to eat and drink. Changes to your diet and medications can be used to treat and lessen the pain caused by mucositis.
- Fatigue: Fatigue is feeling very tired or exhausted. You may feel the need to take a nap. Listen to what your body is telling you and rest when you can.
- Skin irritation: Your skin may become red, irritated, dry, sensitive, and darker in color. It may look or feel like a sunburn. Treat the skin gently to avoid further irritation, and bathe carefully, using only warm water and mild soap. Do not use perfumed or scented lotions or soaps, and avoid sun exposure, as they worsen irritation.
- Alopecia (Hair loss): You will lose some or all of the hair on your body. This includes your head, eyebrows, pubic hair, and legs/arms, etc. The hair usually grows back several months after you finish your treatment.
- Bone marrow suppression: (low blood counts): It is normal for blood counts to become low. The goal of TBI is to suppress the bone marrow so that the body is prepared for the bone marrow/stem cell transplant.
What are the possible long-term side effects of TBI?
Long-term or late side effects of TBI are those that you experience months to years after treatment.
- Cataracts: It is important to visit the eye doctor each year to be monitored for cataracts. You may also have dry eye and using artificial tears can help.
- Pericarditis (Inflammation or swelling of the sac around your heart): Can occur from months to years after TBI. Signs of pericarditis are chest pain, shortness of breath, trouble breathing when you lie down, cough, fever, swelling of your legs, and fatigue.
- Thyroid Issues: TBI can cause thyroid problems, including hypothyroidism (under reactive), hyperthyroidism (overreactive), and thyroid nodules/tumors. During your yearly physical your provider will feel your thyroid for changes, and your primary care provider should ask you to have your blood drawn to see how your thyroid is working.
- Liver Damage: TBI can also cause long-term damage to the liver. Signs of liver damage are abdominal pain, swelling of the abdomen (ascites), weight gain, and/ or yellowing of the skin and eyes (jaundice). If you have any signs of liver problems, you should call your provider right away. Once a year your primary care provider should order blood work to check your liver enzymes. You should also avoid excessive alcohol consumption.
- Kidney Damage: TBI may cause long-term damage to the kidneys. This can result in lower kidney function and high blood pressure. During your yearly physical exam your primary care provider should check your blood pressure and you will have blood drawn to check your kidney function.
- Lung Damage: TBI treatments can cause scarring of your lungs. If you are a smoker or have smoked in the past, seeing a pulmonologist (physician who focuses on lung conditions) can help you manage late side effects from treatment. If you do smoke, you should quit. If you have any new or worsening shortness of breath or cough, you should contact your provider right away.
- Fertility problems: TBI can cause permanent sterility in both men and women. It is important to talk to your care provider before starting radiation about fertility options such as harvesting and freezing eggs and sperm.
If you have any questions or concerns about TBI you should contact your provider.
Resources for More Information
References
Freyer, C. W., Fradley, M., Madnick, D., Carver, J. R., Frey, N. V., Gill, S. I., Ky, B., Luger, S. M., Martin, M. E., McCurdy, S. R., O'Quinn, R., Perl, A. E., Stadtmauer, E. A., & Loren, A. W. (2021). Characterization of Pericarditis following Allogeneic Hematopoietic Cell Transplantation. Transplantation and cellular therapy, 27(11), 934.e1–934.e6. https://doi.org/10.1016/j.jtct.2021.07.025
Leaver, D., Washington, C.M. Principles and Practice of Radiation Therapy, St. Louis, Mosby, 2004.
Sengupta, A., Wilke, D. R., Cherpak, A., Chytyk-Praznik, K., Schella, J., Yewondwossen, M., Allan, J., & Mulroy, L. (2020). Surface Dosimetry of Patients Undergoing Total Body Irradiation: A Retrospective Analysis for Quality Assurance. Cureus, 12(2). https://doi.org/10.7759/cureus.6900