Surgical Procedures: Surgery and Staging for Colon Cancer
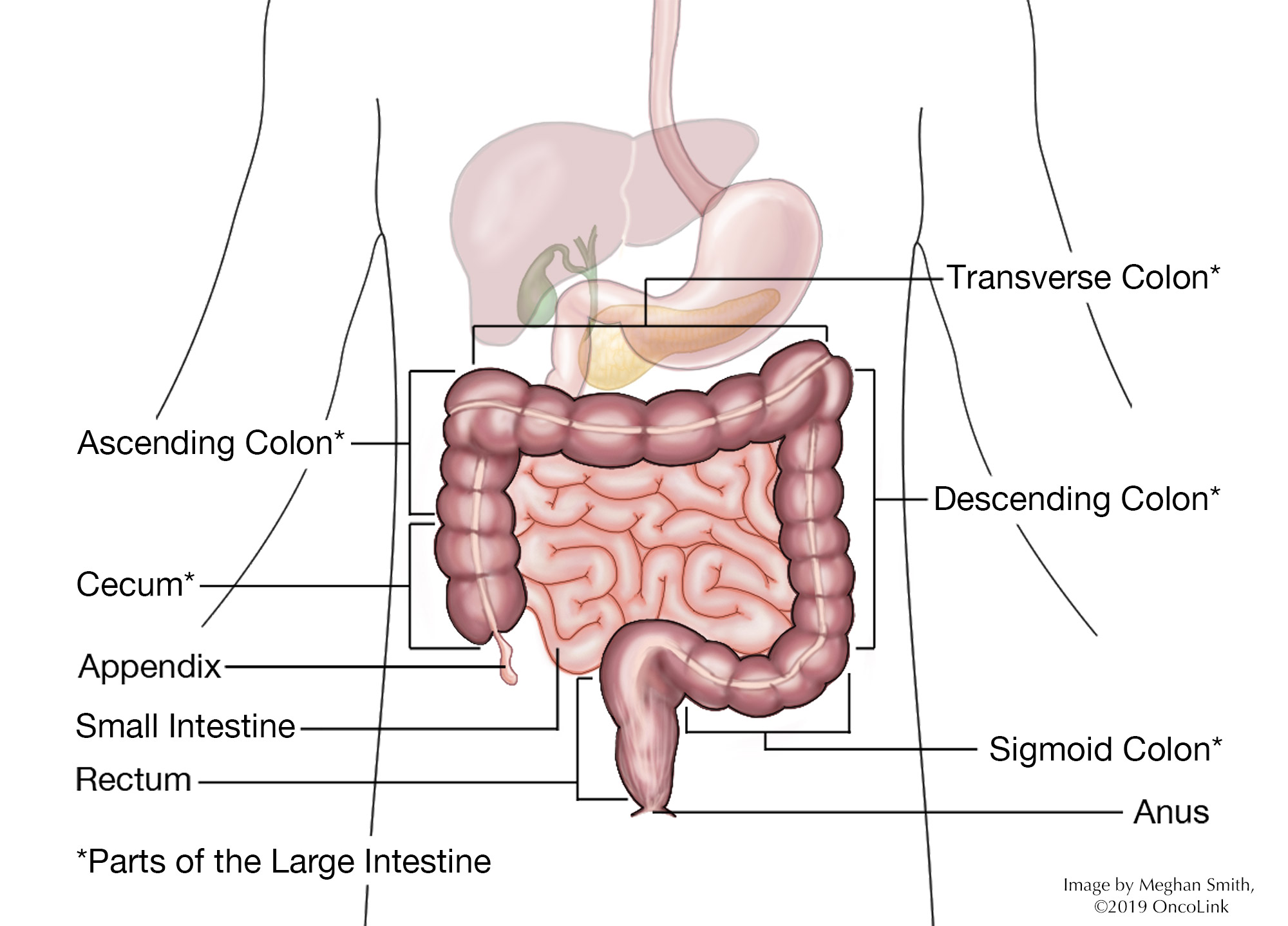
Colon cancer is when cancer cells are found in the colon. The colon, or large bowel, is about 5 feet long. It is part of the body’s digestive system, which breaks down nutrients and gets rid of waste from your body.
Colon cancer often starts in precancerous polyps. These are called adenomatous polyps. These polyps can turn into cancer and spread to the intestinal wall. The most common type of colon cancer is adenocarcinoma. Other types are:
- Carcinoid tumors.
- Gastrointestinal stromal tumors (GISTs).
- Lymphomas.
- Sarcomas.
What is staging and how is it done?
Staging is a way to find out if and where cancer has spread in your body. Your provider will have you get a few tests to figure out the stage of your cancer. These tests may include:
Physical Exam: This is a general exam to look at your body and to talk about your past health issues.
Fecal Occult Blood Testing: Your stool will be checked for blood.A guaiac-based fecal occult blood test (gFOBT) and fecal immunochemical test (FIT) are used.
Stool DNA testing: This test checks for abnormal DNA in your stool.
Laboratory Tests: Blood is drawn to check how your kidneys and liver are working, as well as a complete blood count (CBC). A carcinoembryonic antigen (CEA)level may also be checked.
Imaging: Radiology tests can look inside your body at the cancer and see if it has spread. These tests can include:
- Chest X-ray.
- CAT scan (CT scan).
- Magnetic resonance imaging (MRI).
- Positron emission tomography scan (PET scan).
- Virtual colonoscopy.
Procedures: Each case of colon cancer is different. Talk with your care team about which procedures may be part of your treatment plan. These options may be:
- Colonoscopy: A colonoscope (lighted, flexible tube) is put into the rectum, and looks at the whole colon for anything not normal. Biopsies may be done during a colonoscopy.
- Sigmoidoscopy: A sigmoidoscope (lighted, flexible tube) is put into the rectum and the lower part of the colon (sigmoid colon). It looks for anything not normal. Biopsies can be done during a sigmoidoscopy.
- Double-contrast barium enema: Also known as a lower GI series, this test uses barium (liquid enema contrast) and X-rays to see changes in the lower gastrointestinal tract, including the colon and the rectum.
- Biopsy: A piece of tissue is removed to be looked at under a microscope to look for cancer cells.
Colon cancer spreads to other parts of the body through the tissue, lymph, and blood systems. The stage of your cancer tells how extensive your cancer is, how far it has spread, and what treatment might be best. Colon cancer is described as stages 0 through stage IV (four) disease, with higher stage being more advanced.
Surgical Procedures for Colon Cancer
There are many types of surgery used to treat colon cancer. The type of surgery you have will depend on your health and if the cancer has spread. Some surgeries are:
- Polypectomy/Local Excision: A colonoscope (as in the colonoscopy) removes a polyp or abnormal area of cancer. During a polypectomy, only the polyp is removed. During a local excision (also known as an endoscopic mucosal resection), some of the tissue on the colon wall is also removed.
- Colon resection: The larger cancer is removed by doing a colectomy. There are two types of colectomies:
- Partial colectomy: Also called a hemicolectomy or segmental resection. This procedure removes the cancer and some healthy tissue around the cancer. Lymph nodes may also be removed during this procedure. After this procedure, you will need either an anastomosis or colostomy:
- When the surgeon sews the two ends of the colon back together, this is called an anastomosis.
- Sometimes, a permanent or temporary colostomy or ileostomy is needed. This lets waste (stool) pass through an opening (stoma) on your skin into a colostomy collection bag.
- Total Colectomy: The whole colon is removed. Lymph nodes may also be removed during this procedure. You may need a permanent colostomy to remove waste (stool) from your body.
- Partial colectomy: Also called a hemicolectomy or segmental resection. This procedure removes the cancer and some healthy tissue around the cancer. Lymph nodes may also be removed during this procedure. After this procedure, you will need either an anastomosis or colostomy:
- Laparoscopy: Several small incisions (cuts) are made to let special surgical tools (lighted cameras, cutting tools) pass through to remove any abnormal areas.
- Palliative surgery: The goal of this kind of surgery is not to remove the cancer, but to relieve symptoms and improve your quality of life. Palliative surgery can help with pain caused by the effects of cancer, such as blockages. For example, a diverting colostomy (ostomy placed above the colon tumor) may be done to relieve the symptoms of a blockage.
- Surgery for metastatic disease: At times, colon cancer may spread to other parts of the body, such as the lungs or liver, and these areas may need to be removed.
- Radiofrequency ablation: Electrodes kill cancer through a probe placed through the skin or an abdominal (belly) incision.
- Cryosurgery: Abnormal cells are frozen and killed.
What are the risks of colon cancer surgery?
As with any surgery, there are risks and possible side effects. These can be:
- Reaction to anesthesia (Anesthesia is the medication you are given to help you sleep through the surgery, to not remember it, and to manage pain. Reactions can include wheezing, rash, swelling and low blood pressure).
- Bleeding.
- Blood clots.
- Infection.
- Pneumonia (lung infection).
- Fistula formation (abnormal hole).
- Nearby organs like the intestines, bladder, blood vessels, and ureter, can be affected.
- New adhesions or scar tissue.
- Bowel obstruction (blockage).
- Incisional hernia.
- Anastomotic leak (leakage from the joined colon or anastomosis site).
What is recovery like?
Recovery from colon cancer surgery depends on the procedure you’ve had. Most often, a 3-4 day hospital stay is needed.
You will be told how to care for your incisions before you go home. 4Your medical team will talk with you about the medications you will be taking, such as those for pain, blood clot, infection, and constipation prevention, or other side effects. Your healthcare provider will talk with you about changes in your activity level depending on the surgery you have had.
Often, after a colectomy, you will be told:
- No heavy lifting (anything over 10 pounds) for 4 to 6 weeks after surgery.
- Try not to strain while having a bowel movement.
- Take all medications as told.
- Go back to your normal activities within 1-3 weeks. This could include work (depending on your type of work), light physical activity, driving, walking up stairs, and sexual activity when advised.
- Do not drive while taking narcotic medications.
- Shower instead of taking a bath. Do not tub bathe until your provider tells you that you can.
- Advance your diet as told. You may be asked to eat a low-residue diet for 4 weeks after surgery.
- Drink 8 to 10 glasses of water per day unless otherwise told to do so.
Call your healthcare team if you have:
- If your pain gets worse or does not get better with your pain medications.
- Fever. Your care team will tell you at what temperature to call them.
- Swelling, vomiting that doesn’t stop, abdominal pain that gets worse.
- Signs of infection like incisional redness, swelling, bleeding, or drainage.
- Lack of bowel movement for 2 to 3 days.
- Any other concerns or questions you may have.
What will I need at home?
- Thermometer to check for fever, which can be a sign of infection.
- Loose clothes and underwear.
- Incision and/or ostomy care items. These are often supplied by the hospital/your care provider’s office.
How can I care for myself?
You may need a family member or friend to help you with your daily tasks until you are feeling better. It may take some time before your team tells you that it is ok to go back to your normal activity.
Be sure to take your prescribed medications as directed to prevent pain, infection and/or constipation. Call your team with any new or worsening symptoms.
There are ways to manage constipation after your surgery. You can change your diet, drink more fluids, and take over-the-counter medications. Talk with your care team before taking any medications for constipation.
Taking deep breaths and resting can help manage pain, keep your lungs healthy after anesthesia, and promote good drainage of lymphatic fluid. Try to do deep breathing and relaxation exercises a few times a day in the first week, or when you notice you are extra tense.
- Example of a relaxation exercise: While sitting, close your eyes and take 5-10 slow deep breaths. Relax your muscles. Slowly roll your head and shoulders.
This article contains general information. Please be sure to talk to your care team about your specific plan and recovery.
References
National Cancer Institute. Colon Cancer Treatment (PDQ®)–Patient Version. 2020. Found at: http://www.cancer.gov/types/colorectal/patient/colon-treatment-pdq.
Mayo Clinic Staff. Colon Cancer. 2019. Found at: http://www.mayoclinic.org/diseases-conditions/colon-cancer/home/ovc-20188216
American Cancer Society. What is Colorectal Cancer? 2020. Found at: http://www.cancer.org/cancer/colonandrectumcancer/detailedguide/colorectal-cancer-what-is-colorectal-cancer
The University of Chicago Medicine. Frequently Asked Questions About Colectomy (Colon Resection) Found at: http://www.uchospitals.edu/specialties/colorectal/services/colectomy.html#P75_10158