Brachytherapy for Prostate Cancer
What is brachytherapy?
Brachytherapy is radiation therapy that is given inside the body. Radioactive material is put either into or near the tumor. The material may be left in your body or taken out. The tissues closest to the radioactive material get the most radiation. The tissues further away get less radiation. Brachytherapy is used to treat some cases of prostate cancer.
Compared to external beam radiation, brachytherapy:
- Often causes less harm to healthy tissues.
- Delivers a higher dose of radiation in a shorter amount of time.
Types of Brachytherapy for Prostate Cancer
Brachytherapy is most often used for prostate cancer that has not moved outside of the prostate gland or the area around it. It may be used with traditional (external beam) radiation when the cancer is more advanced to give even higher doses of radiation to the prostate.
Prostate cancer can be treated with low dose rate (LDR) brachytherapy or high dose rate (HDR) brachytherapy.
Low Dose Rate (LDR) Brachytherapy Procedure
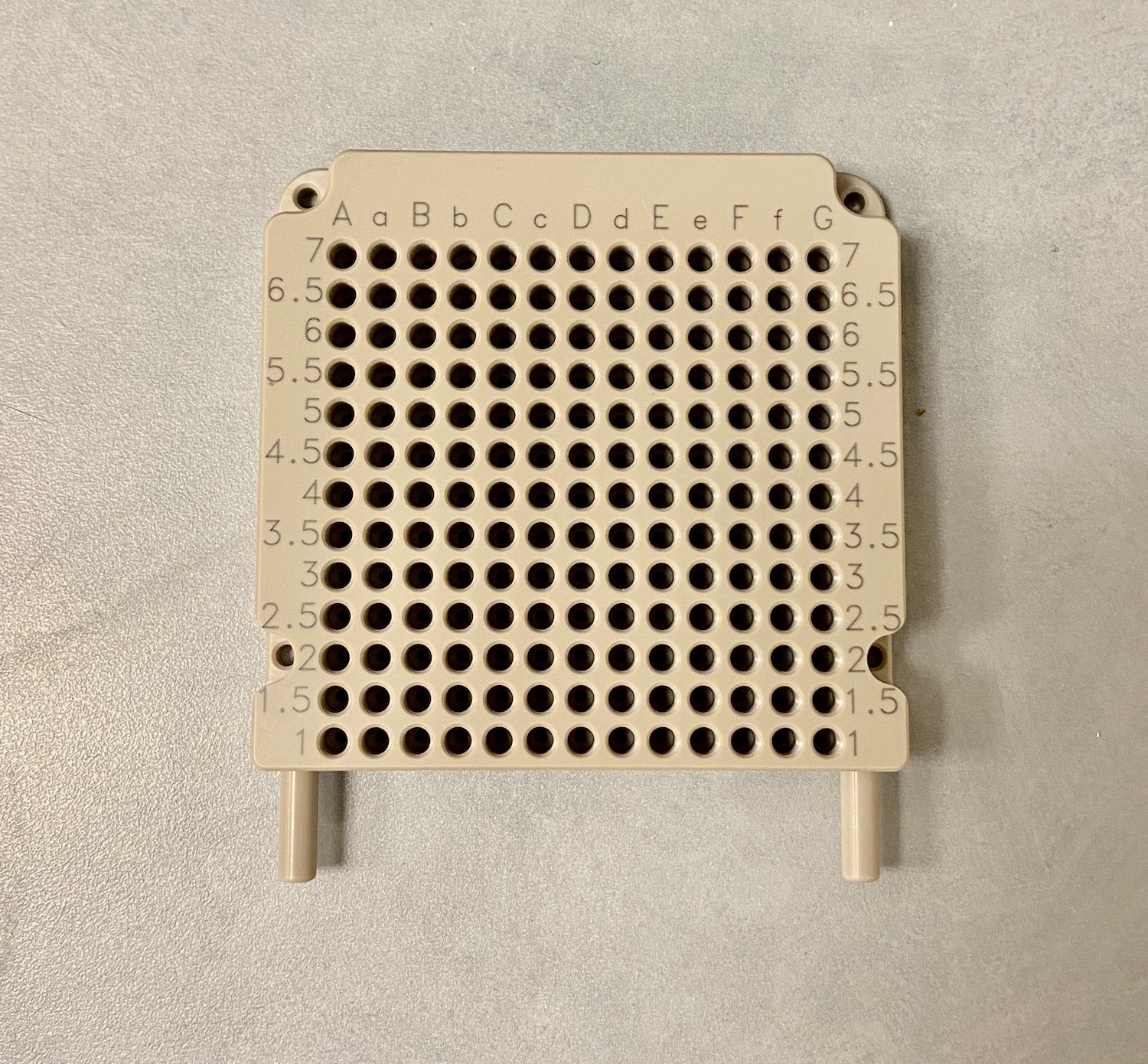
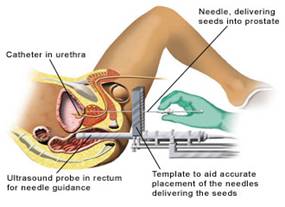
LDR brachytherapy may also be called seed therapy, seed implantation, or permanent brachytherapy. It is done in the operating room, and you are usually given general anesthesia (anesthesia is the medication you are given to help you sleep through the surgery, to not remember it, and to manage pain). While you are asleep, a temporary urinary catheter is placed to empty your bladder (remove all of the urine). Thin needles are placed through the perineum skin (the area between the anus and the scrotum) into the prostate, using ultrasound imaging and a template (small grid) to guide them. The radioactive seeds are inserted through the needles and into the prostate. The needles are taken out, leaving the seeds behind, spaced throughout the prostate. The seeds are not taken out (stay in the prostate). The number of seeds depends on the size of the prostate gland, ask your provider how many were placed. The seeds slowly release radiation into the tissue around them, over many months, killing the cancer cells.
You will go home after you wake up and spend a short time in the recovery room. Because of the seeds, your provider may tell you to:
- Limit close contact with children and pregnant women.
- Not have children sit on your lap for long periods.
- Not have sexual intercourse for some time.
- Use a condom during sexual intercourse in case a seed is passed in your semen.
There is also a small risk of the seeds getting out of the prostate and moving to somewhere else in the body such as the chest, abdomen, or pelvis. This is very rare, and your provider will let you know if the seed needs to be retrieved if it were to move outside the prostate.
High Dose Rate (HDR) Brachytherapy Procedure
HDR brachytherapy is also called remote afterloading brachytherapy or temporary brachytherapy. This procedure is often done in the operating room with general anesthesia (anesthesia is the medication you are given to help you sleep through the surgery, to not remember it, and to manage pain). Hollow needles are placed through the perineum skin (the area between the anus and the scrotum), and into the prostate. In some cases, a template (small grid) can be used to help guide the needles. An ultrasound probe is placed in the rectum to make sure the needles are placed correctly.
While you are asleep, a temporary urinary catheter is placed to empty your bladder (remove the urine). Also, while you are asleep, the needles are adjusted (moved) and ultrasound images are taken. These images are used to plan your treatment, called ultrasound-based HDR prostate brachytherapy. Your treatment plan will be made to treat the prostate gland and cancer. A CT scan or MRI may also be done to help make your treatment plan.
Some clinics wake you up once the catheter and needles are in place while other clinics keep you asleep throughout the entire treatment.
Once the treatment plan is ready, the brachytherapy machine is connected to the catheters. The machine pushes the radioactive source into the catheters one by one, then removes it based on the treatment plan. The amount of time the source stays in one spot is called the ‘dwell time’. The dwell time is programmed to make sure the planned dose is given to the prostate. It is also made to ensure other body parts, like the urethra, rectum, and bladder, get as little radiation as possible.
To prevent exposure to others, no one is allowed in the treatment room while the source is out of the machine and inside the patient. After the treatment, the radioactive source is removed from your body, and you are not radioactive. The needles and the urinary catheter are also removed. Depending on your type of prostate cancer, you may have this procedure repeated once more after a 1–2-week break.
What are the side effects?
Side effects can include pain or swelling in the perineum. You may have burning and hesitancy with urination due to the urinary catheter, which can last up to 2 weeks. Long-term side effects that last months to years after treatment may include:
- Burning with urination.
- Urinary incontinence (not being able to hold your urine).
- Urgent bowel movements.
- Diarrhea.
- Rectal bleeding.
- Erectile dysfunction (not being able to get or maintain an erection).
Choosing Your Treatment
Not all prostate cancers can be treated with brachytherapy. You should talk to your provider about what treatment is best for you. It is important to talk about possible side effects from each treatment, as these can depend on your age and overall health. Each treatment has different recovery times as well. These things may help you decide which treatment is best for you.