Breast MRI
What is a breast MRI?
Magnetic Resonance Imaging, also called MRI, is a radiology test that uses strong magnets and radiofrequency waves to make a detailed picture of bones, soft tissues (muscles, tendons, etc), organs and other parts of the body. The test does not use any radiation. A breast MRI is an MRI done with a special machine that has tools to make detailed pictures of the breasts.
What is breast MRI used for?
Breast MRI can help providers learn more about the health of your breasts and can help find issues that cannot be seen on a mammogram or ultrasound. MRI should not replace a mammogram and the tests are often used together. Each test can find different issues in your breast tissue. Some providers suggest alternating the tests every six months, while others see a benefit to reading them together. Your provider will be able to tell you when you should have each test.
Breast MRI has many uses, such as:
- Breast cancer screening for women at high risk of breast cancer due to family history or their own health history.
- To check findings from a mammogram that need further testing.
- To evaluate a new cancer diagnosis.
- As a follow-up after treatment for breast cancer.
- To check breast implants that may have broken.
How do I prepare for the test?
There is usually no special preparation for a breast MRI. Unless you are told not to, you can eat and drink as you normally would. It is best to leave jewelry, body piercings, hair clips, and other metals at home, as these are not allowed in the MRI room. Let the technician know if you have any metal in your body, such as a defibrillator/pacer, port-a-cath, or other metal implants.
If you are claustrophobic (do not like confined spaces), you may need to take medication to help you relax before the test. Talk with your healthcare provider if you have any concerns.
How is the test performed?
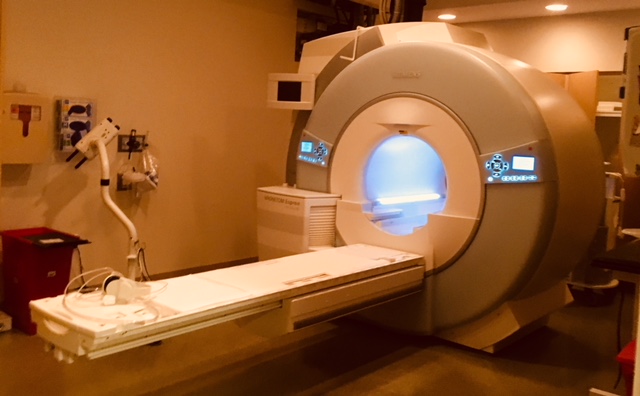
A breast MRI uses a table with holes in it for your breasts. You will lie face down on the table, with your breasts hanging through the holes. This allows the breast tissue to be looked at without being squeezed, like in a mammogram. The machine may press against your breasts to keep them from moving. You will need to lie still for the test, so it is important that you are comfortable. The table slides into a tube, with the magnets spinning around you. The MRI is loud, so you may be given headphones or earplugs to help block out the noise.
Breast MRI almost always uses a contrast (dye) given into a vein (IV) called gadolinium. You will not have contrast if the MRI is looking for ruptured implants. The contrast will be given before the test. The whole test can take 45-60 minutes.
What is a fast breast MRI?
The fast breast MRI, also called an abbreviated breast MRI, is sometimes used along with a mammogram for women with dense breast tissue who do not meet the requirements for a full breast MRI. It cannot find as much as a full breast MRI, but it is good at finding invasive breast cancer. The test can be done in as little as 10-15 minutes. Many health plans do not pay for this test. You may have to pay out-of-pocket for the test, which typically costs around $300-400.
Who should have a breast MRI?
Women at high risk of breast cancer should have a breast MRI. The American Cancer Society (ACS) breast cancer screening guidelines suggest yearly screening MRI, along with mammogram, for the following women:
- Those with a known BRCA 1 or 2 (genetic) mutation.
- Women who have not had genetic testing, but have a first-degree relative with a BRCA mutation (sister, mother, daughter).
- Women with a predicted lifetime risk of 20% to 25% or greater of breast cancer (determined by using risk assessment tools - more below).
- Women who received radiation to the chest between the ages of 10 to 30.
- Women with certain genetic syndromes, or a first-degree family member with the syndrome (Cowden, Li-Fraumeni, Bannayan).
Some women are considered high risk for breast cancer but are not a part of the above groups. These include women with:
- Predicted lifetime risk of less than 20%, but more than 15%.
- Those with a history of lobular carcinoma in situ (LCIS), atypical lobular or ductal hyperplasia.
- High breast density (dense breast tissue) on a mammogram.
Ask your provider if and when you should have a breast MRI. You can also learn more about your risk of breast cancer here:
What about cost?
An MRI is more costly than a mammogram. Coverage by insurance companies will differ and will likely depend on the woman's risk. Be sure to check on your coverage with your insurance company before having a breast MRI.
Not all clinics have breast MRI machines and providers who can read the results. It is important to talk to your provider about if this is a test you should have and where to have it done.