Surgical Procedures: Surgical Staging for Vaginal Cancer
What is surgical staging and how is it done?
Cancerous cells in the vagina are called vaginal cancer. The two most common types are squamous cell carcinoma and adenocarcinoma. Once a diagnosis of vaginal cancer has been made, you will need testing to figure out the stage (extent) of your cancer. These tests are:
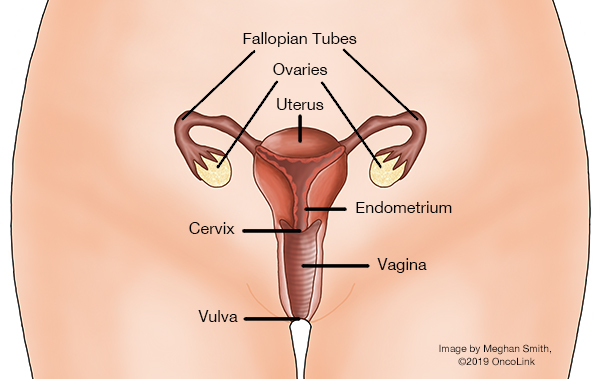
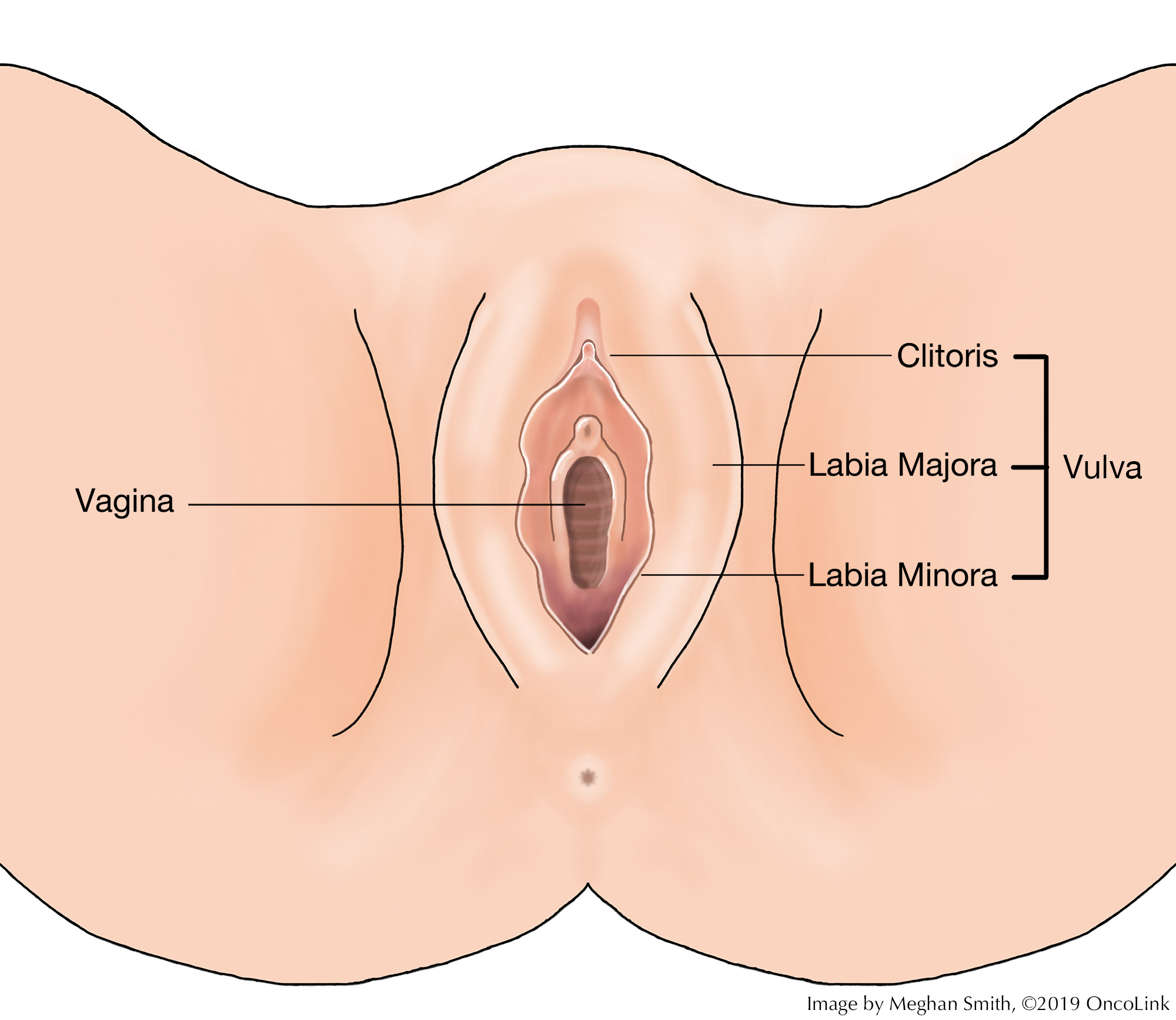
- Pelvic Exam: Your healthcare provider will check your pelvic organs, such as the vagina, cervix, uterus, fallopian tubes, ovaries, and rectum, for any changes. The exam is done with a speculum and gloved fingers. A general physical exam and medical history will also be done.
- Pap Smear: A sampling of the vagina and/or cervix cells will be taken with a pap smear, using a brush, cotton swab, or spatula.
- Colposcopy: A lighted magnifying tool, called a colposcope, is used to look at the tissues of the vagina and cervix to check for any abnormalities.
- Cystoscopy: A cystoscope, a tube with a light on the end of it, is used to look at the bladder and urethra to check for any changes.
- Ureteroscopy: A ureteroscope, a tube with a light at the end of it, is used to look at the ureters and check for any changes.
- Proctosigmoidoscopy: The rectum and part of the colon are looked at to see if the cancer has spread.
- Radiologic Imaging: Imaging such as X-rays, CT scans, Magnetic Resonance Imaging (MRI), and Positron Emission Tomography (PET Scan) may be used to further check the extent of your cancer.
Vaginal cancer spreads to other parts of the body through the tissue, lymph, and blood systems. Cancer stage tells you how extensive the cancer is, how far it has spread, and what treatment course will be recommended. Healthcare providers will use two staging systems to tell the stage of your cancer, the FIGO staging system (International Federation of Gynecology and Obstetrics) and the American Joint Committee on Cancer TNM staging system. Both staging systems tell your healthcare team information on the extent of the tumor (T), spread to the lymph nodes (N), and distant metastasis (spread) (M).
Surgery can be used to treat vaginal cancer. There are many types of surgical procedures used, based on your stage and situation.
Surgical options for vaginal cancer are:
- Laser: A laser beam is used to remove (take out) pre-cancerous lesions in the vagina.
- Wide Local Excision: The cancerous lesion, as well as some surrounding normal tissue, is removed.
- Vaginectomy: Removal of the vaginal tissues.
- Partial Vaginectomy: Part of the vagina is removed.
- Total Vaginectomy: Removal of the whole vagina.
- Radical Vaginectomy: Removal of the whole vagina and some surrounding tissue.
- Trachelectomy: In cases where the cancer is near the cervix, the uterus may be left in place while the cervix is removed. This can allow for fertility preservation.
- Hysterectomy: (may also need a vaginectomy)
- Total Hysterectomy: Removal of the uterus and cervix. In some cases, the ovaries and fallopian tubes will stay in place.
- Radical Hysterectomy: Removal of the uterus, cervix, tissue surrounding the cervix, and the upper part of the vagina. The fallopian tubes may/may not be removed.
- Lymph Node Dissection: Removal of lymph nodes that are in the groin and or pelvis to check for cancer.
- Pelvic exenteration: Removal of a woman’s uterus, cervix, ovaries, fallopian tubes, vagina, and at times, the bladder, urethra, and/or bowel, anus, and rectum.
Drains may be placed to remove extra fluid from the surgical area. You may have these for a short time and will be removed in your provider’s office. You will be taught how to care for the drains. Some vaginectomy sites will need a skin graft. A skin graft is taking skin from another part of the body to close the wound. For women who have undergone an extensive vaginectomy, reconstructive surgery is an option.
What is recovery like?
Recovery from surgery for vaginal cancer will be based on many factors. You will likely stay in the hospital for one to a few days, based on the type of procedure you have had.
Your medical team will tell you the medications you will be taking for blood clots, constipation and infection prevention, and pain management.
Your healthcare provider will talk to you about restrictions, which depend on the surgery you have had.
How can I care for myself?
You may need a family member or friend to help you with your daily tasks until you are feeling better. It may take some time before your team tells you that it is ok to go back to your normal activity.
Be sure to take your prescribed medications as directed to prevent pain, infection, and/or constipation. Call your team with any new or worsening symptoms.
There are ways to manage constipation after your surgery. You can change your diet, drink more fluids, and take over-the-counter medications. Talk with your care team before taking any medications for constipation.
Taking deep breaths and resting can help manage pain, keep your lungs healthy after anesthesia, and promote good drainage of lymphatic fluid. Try to do deep breathing and relaxation exercises a few times a day in the first week, or when you notice you are extra tense.
- Example of a relaxation exercise: While sitting, close your eyes and take 5-10 slow deep breaths. Relax your muscles. Slowly roll your head and shoulders.
This article contains general information. Please be sure to talk to your care team about your specific plan and recovery.