All About Neutropenia
What are white blood cells?
A white blood cell (WBC) is one type of blood cell in the body. These cells are part of our immune system. Our immune system fights infection and protects our bodies from harmful bacteria, viruses, and other foreign invaders. WBCs are made in the bone marrow. They are found in our blood and lymph systems. There are five types of white blood cells. Each has its own job in the immune system:
- Neutrophils (50-70% of the WBCs).
- Lymphocytes (T and B cells) (25-35%).
- Monocytes (4-6%).
- Basophils (0.4-1%).
- Eosinophils (1-3%).
To check the number of each of these white blood cells, you will have a Complete Blood Count (CBC) blood test with differential. Your provider may also check your Absolute Neutrophil Count (ANC) which is the number of neutrophils. This article will focus on the role of neutrophils and what happens when they are low.
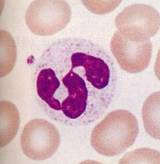
What is a neutrophil?
- Neutrophils make up the largest number of WBCs.
- They quickly go to an infection, take in, and kill foreign particles.
- They can be found in the pus of a wound and play a role in acute inflammation (redness, warmth, swelling, and pain).
- Mature neutrophils are sometimes called "segs,” named for their segmented (broken up) nucleus.
- Immature neutrophils are called "bands" because their nucleus appears banded.
- These mature segs and immature bands both make up the ANC.
What is neutropenia?
- A normal ANC is between 2,500 and 5,000.
- A low neutrophil count is called “neutropenia.” Neutropenia means an ANC of less than 1,500.
What causes neutropenia?
Neutropenia can be caused by:
- Cancer that affects the bone marrow or an immune disorder.
- Cancer medications like chemotherapy and targeted therapies.
- Radiation therapy harming the bone marrow that makes these blood cells.
- Other medications like anti-thyroid medicines, certain antibiotics, some blood pressure medicines, and more.
Why do cancer therapies cause neutropenia?
Cancer therapies like chemotherapy, biotherapy, and radiation therapy cannot tell the difference between cancer cells and healthy cells. Most chemotherapies work by killing cells that divide quickly. Cancer cells divide quickly, but so do blood/bone marrow cells like WBC, hair follicles, and the cells that line the gastrointestinal (GI) tract (mouth, throat, stomach, and bowel). When these normal cells are harmed, you may have side effects like low blood counts, hair loss, mouth sores, and diarrhea. Radiation harms blood cells by affecting your bone marrow (where blood cells are made) in the area where you are being treated.
Why is neutropenia important?
A low neutrophil count increases the risk of getting an infection. When bacteria goes into the body, there are not enough neutrophils to fight it off. The lower the ANC, the higher your risk of getting an infection.
Grades of Neutropenia
- Mild Neutropenia: An ANC between 1,000 and 1,500. Minimal risk of infection.
- Moderate Neutropenia: An ANC between 500 and 1,000. Moderate risk of infection.
- Severe Neutropenia: An ANC less than 500. Severe risk of infection.
What is a nadir?
Nadir is a term you might hear your healthcare team use. Nadir is the point after treatment when your blood counts are at their lowest. This can include white blood cells, red blood cells, and/or platelets, based on the type of treatment you had and your body's response. This decrease in blood counts is also called “myelosuppression.”
Nadir often occurs 7-10 days after chemotherapy. Your blood counts will then slowly climb back before the next treatment. If your blood counts have not come back up enough, your healthcare team may delay your next therapy. Giving you more therapy with blood counts that are too low could make it very hard for your body to recover.
What can I do to avoid infection?
Washing your hands is the best way to prevent infection. This includes you and all other members of your household. If you are around small children, teach them to wash their hands. Avoid large crowds, like the mall during the holidays. Avoid people you know are sick with things including colds, viruses, or other infections. It is also a good idea to avoid people who live in a house with other people who are sick, even if they themselves do not feel sick.
Know the signs of an infection including: a high fever, redness, swelling, or pus. These signs are caused by neutrophils, but when you are neutropenic you don’t have enough neutrophils to cause these signs. When neutrophils and other blood counts are low, you must take even the most minor signs seriously and call your healthcare team right away, day or night! A temperature of 100.4°F (38°C) or higher can be very dangerous for a person on treatment. Make sure you know the number to call so you can reach your care team at all times, especially after hours (night and weekends), if you have a fever or other problems.
Signs of infection to watch for:
- Temperature > 100.4°F (38°C).
- Shaking chills.
- Cough, sore throat.
- Burning when you pee (urinate).
- New lower back pain.
- Blood in pee (urine).
- Diarrhea or loose stool.
- Rash.
- Redness, soreness around central line catheter, or a wound.
Can you prevent neutropenia?
A group of medications, called growth factors, or colony-stimulating factors, can help prevent neutropenia or help shorten the length of time you are neutropenic. Your healthcare provider may prescribe one of these medications. There are a few growth factors available in the United States: filgrastim (Neupogen®), pegfilgrastim (Neulasta®), and sargramostim (Leukine®). These are manmade versions of a protein produced in the body that helps you make more neutrophils.
These medications are given as a subcutaneous (SubQ) injection (a shot given just under the skin). These medications are started no earlier than 24 hours after chemotherapy. In the case of filgrastim and sargramostim, they are given once a day until after the nadir and the ANC returns to a normal level. In the case of pegfilgrastim, only one injection is required, given 24 hours after chemotherapy. There is also a version of pegfilgrastim (On-Pro) that is a patch put on your arm by your provider that automatically gives you the injection the next day at the correct time.
Why is it important to prevent neutropenia?
Your healthcare team has created a specific treatment plan and treatment schedule for you. Neutropenia can cause delays in treatment and dose reductions (receiving a lower dose), which can make your treatment less effective. Studies show that for certain types of cancer, cancer therapies give the best long-term results when patients get the full dose on time, every time. Preventing neutropenia gives you a better chance of being able to stick to your treatment schedule which is important for treating your cancer.
What else should I know?
Ask your healthcare team about your blood counts and record them in a log. Know the signs of infection and who to tell if you develop any. If you have neutropenia, ask about using a growth factor for future cycles of chemotherapy. Teach those around you how they can help keep infections away, like by washing their hands or staying home when they feel sick.
Other Resources
Blood counts log: print this log to keep track of your blood counts and treatments.
OncoLink Rx: learn about the medications you are receiving.
Neutropenia Tip Sheet: Here you will find helpful tips about infection and cancer-related neutropenia.