Surgical Procedures: Surgery and Staging for Parathyroid Cancer
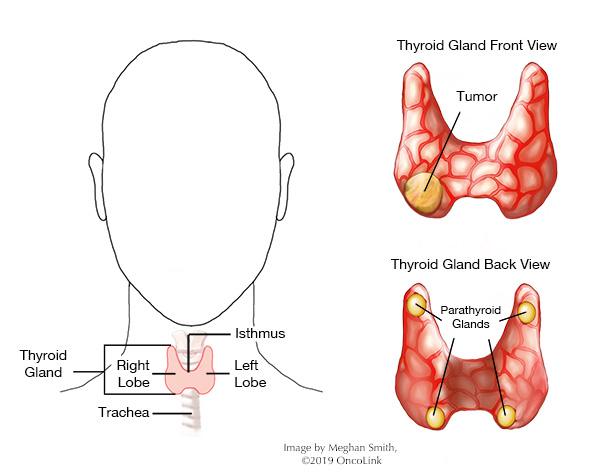
When there are cancer cells in your parathyroid gland, it is called parathyroid cancer. This rare cancer affects the small, pea-sized parathyroid glands found behind your thyroid gland. Your parathyroid gland makes the parathyroid hormone. This gland also stores and uses calcium in your body.
You may be at a higher risk of parathyroid cancer if you have certain genetic disorders, like familial isolated hyperparathyroidism (FIHP) or multiple endocrine neoplasia type 1 (MEN1) syndrome.
Note: Malignant (cancerous) cells can look like a benign (noncancerous) parathyroid adenoma, making it hard to diagnose parathyroid cancer. Your provider will look at your symptoms, blood calcium level, parathyroid hormone levels, and tumor to diagnose your cancer.
What is staging and how is it done?
Staging is a way to find out if and how far the cancer has spread in your body. Your provider will have you get a few tests to figure out the stage of your cancer. For parathyroid cancer, these tests may be:
Physical Exam: This is an exam to look at your body and talk about past health issues.
Serum Markers: Blood samples may be taken to check calcium and parathyroid levels. You may need venous sampling, where blood samples are taken from specific veins in your body.
Imaging: Radiology tests can look inside your body to look at the cancer and see if it has spread. These tests can include:
- CAT scan (CT scan).
- Ultrasound.
- Single Photon Emission Computed Tomography (SPECT scan).
- X-Ray.
- Magnetic resonance imaging (MRI).
- Bone Density Testing.
- Angiogram.
- Sestamibi Scan (a nuclear medicine scan to check paraythroid glands).
Other: Your provider may recommend other tests to check for parathyroid cancer, including urine tests.
Parathyroid cancer spreads to other parts of the body through the tissue, lymph, and blood systems. Cancer stage determines how extensive the cancer is, how far it has spread, and what your treatment plan should be.
Parathyroid cancer does not have a standard staging process. It is described as localized (in one area) or metastatic (spread to other parts of the body).
What types of surgery are used to treat parathyroid cancer?
Surgical procedures used to treat parathyroid cancers are:
En Bloc Resection: Also called a parathyroidectomy, an en bloc resection removes the whole parathyroid gland, the surrounding capsule (tissue around it), and if needed, half of the thyroid that the cancer is found in, as well as muscles, tissues, and nerves. This can be done as an open procedure with an incision (surgical cut) in the neck or as a minimally invasive procedure using a fiber-optic scope (very small incisions).
Tumor Debulking: As much of the tumor as possible is removed. The whole tumor may not be able to be removed.
Metastasectomy: A metastasectomy is a procedure to remove cancer that has metastasized (spread) to other parts of the body.
With each of these surgeries, the main goal is to have “clean margins.” This means that the edges of the tissue that were removed are free of cancer cells when looked at under a microscope. Your surgeon will try to remove enough tissue so that the margins do not have cancer in them. Having these “clean margins” lowers the risk of cancer growing back (recurrence).
What are the risks of parathyroid surgery?
As with any surgery, there are risks and possible side effects. These can be:
- Bleeding.
- Cardiovascular (heart) issues, such as a heart attack.
- Blood clots.
- Wound infections.
- Chest infections, like pneumonia.
- Low calcium levels.
- Hypothyroidism if your thyroid gland was also removed.
- Keloid (thick scar tissue) formation.
- Numbness at your incision or under your chin that goes away.
- Lump in your throat or throat pressure that goes away.
- Itching at your incision.
- Neck stiffness, tightness, pulling.
- Chest discomfort.
- Headache, ear pain, and/or congestion.
- Hoarse/weak voice and/or pitch/tone changes that go away. Permanent hoarseness may happen when there is injury to the recurrent laryngeal nerve (a nerve in your neck).
- Emotional changes that get better over time, including depression, irritability, fatigue, and/or weakness.
Some people are at a higher risk for side effects and/or surgical complications. Speak with your providers if you have concerns about your surgical risks and possible side effects.
What is recovery like?
Your team will decide if you need to stay in the hospital and for how long. You will be told how to care for your surgical incision before leaving the hospital. Most times, you can return to normal activities within 1 to 2 weeks.
Your care team will talk with you about the medications you will be taking, such as those for pain and/or to treat hypothyroidism, as well as any activity changes you may have to make.
Common instructions after parathyroid surgery are:
- Showering is usually allowed 48 hours following surgery. Pat the incision dry after a shower. Let the steri-strips to fall off or remove them by day 10 to 14.
- Avoid swimming or tub soaking for 2 weeks.
- Avoid driving until you are not taking pain medication and can turn your neck side to side, usually within 1 to 2 weeks after surgery.
- If you have temporary (short-term) throat discomfort or swallowing problems, eat soft foods or easily-swallowed foods/drinks like juice, soup, applesauce, and scrambled eggs.
Call your care team if you have:
- Fever or signs of an infection like chills, redness, tenderness, and/or drainage at the incision. Your care team will tell you at what temperature you should call them.
- Any feelings of dizziness or if you are lightheaded.
- Shortness of breath/having a hard time breathing.
- Nausea/vomiting.
- Numbness/tingling in the hands, feet, and/or mouth.
- Muscle spasms.
How can I care for myself?
You may need a family member or friend to help you with your daily tasks until you are feeling better. It may take some time before your team tells you that it is ok to go back to your normal activity.
Be sure to take your prescribed medications as directed to prevent pain, infection and/or constipation. Call your team with any new or worsening symptoms.
There are ways to manage constipation after your surgery. You can change your diet, drink more fluids, and take over-the-counter medications. Talk with your care team before taking any medications for constipation.
Taking deep breaths and resting can help manage pain, keep your lungs healthy after anesthesia, and promote good drainage of lymphatic fluid. Try to do deep breathing and relaxation exercises a few times a day in the first week, or when you notice you are extra tense.
- Example of a relaxation exercise: While sitting, close your eyes and take 5-10 slow deep breaths. Relax your muscles. Slowly roll your head and shoulders.
*This article contains general information. Please be sure to talk to your care team about your specific plan and recovery.