Total Skin Electron Beam Therapy
What is Total Skin Electron Beam Therapy?
Total skin electron beam therapy (TSEBT) is a radiation treatment for the whole surface of your skin. It is used to treat cutaneous T-cell lymphoma (CTCL) and/or mycosis fungoides (MF), a type of lymphoma that affects the skin.
In TSEBT, a type of radiation is used, called electrons. This beam goes into the first 1-2 centimeters of your body. This treats the skin while limiting radiation to other tissues and organs.
How does TSEBT work?
In standard radiation treatments for cancer, multiple radiation beams enter the body from different angles. These pass through the tumor inside, and then go through, exiting on the other side of the body. All tissues in the path of the beams are exposed to radiation, which can lead to side effects. If we were to treat the whole skin surface like this, the whole body (including all internal organs) would be exposed to radiation. This could cause many side effects.
How is TSEBT given?
Treatments are often given 2-4 days a week, for anywhere from 8-10 weeks. You may be in the treatment room for 30-60 minutes each day. Much of this time is used to get you in the correct positions for treatment. The actual radiation treatment only takes a few minutes. The schedule depends on:
- The dose being given.
- The protocols used by the radiation center where you are being treated.
- The radiation machine being used.
There are a few treatment methods that can be used based on your treatment center.
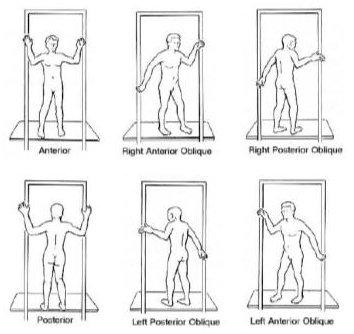
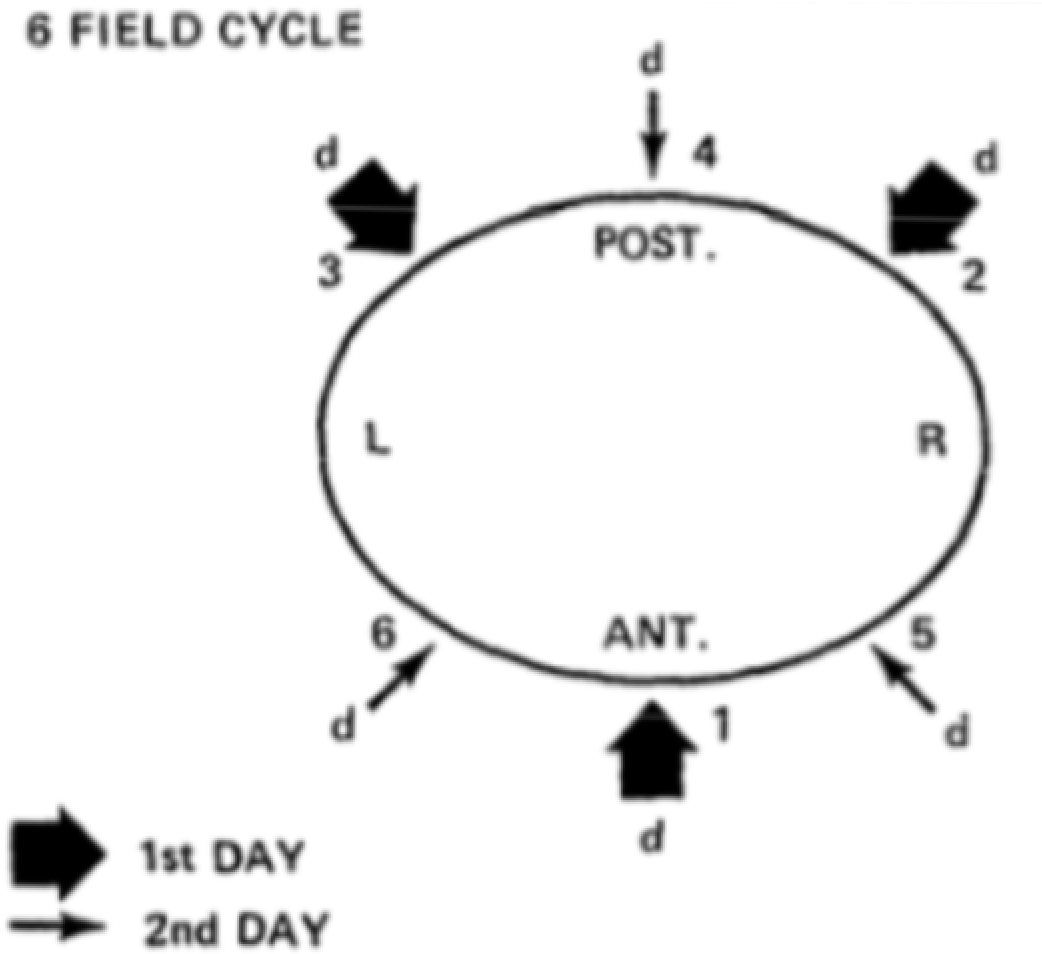
- Stanford Technique vs. Platform: You will either be put in a series of poses (Stanford Technique), or you will stand still on a platform that spins. Both methods will make sure that all areas get the correct dose of radiation.
- One beam vs. Two Beams: Either one beam will be used to treat your body all at once or the beam will be split in two and the top and bottom half will be treated separately.
Certain areas of your body, such as your eyes and nails, will be protected from the radiation with goggles and/or shields. The areas protected may change from day to day.
Other areas of the body, like the soles of the feet, and the perineum (area between the anus and testicles in men and the area between the anus and vagina in women) are treated separately. This is because they are not well exposed during the treatment.
What should I expect during treatment?
During the treatment, your therapists will leave the room. They can see you, hear you, and speak to you through a microphone from a control room. You may hear noises from the machine, but you will not feel the radiation. The treatment is painless.
You will not be wearing clothes and you will stand in front of the radiation machine, which is a few feet away. You may be standing in a box or an enclosed area. This allows the radiation therapists to use pieces of equipment to shield certain areas of your body from the radiation.
If you are being treated using the Stanford Technique, the therapists will come into the treatment room twice to help you change how you are standing. It can be uncomfortable standing in the same position for a long time. Let your therapists know if you are having trouble.
In some cases, after TSEBT treatment, your radiation oncologist may want to give some areas of the skin an extra dose of radiation. This is called a “boost.”
What is spot treatment?
Not everyone needs all of their skin surface treated. If you only need one or a few areas treated, but not the whole body, spot treatment may be used.
Short-Term Side Effects
Some of the most common short-term side effects of TSEBT are:
- Skin irritation: Your skin will become red, irritated, dry, and darker in color. It may look or feel like a sunburn. This begins a few weeks into treatment and often gets better a few weeks after treatment is done. Your skin may stay redder, darker, and drier than it was before treatment. Do not use perfumed lotions or soaps or band-aids. Try not to shave or scratch your skin or go out in the sun. Be sure to always use sunscreen and seek shade when you are outdoors. Wearing soft or loose-fitting clothing may be more comfortable.
- Alopecia (Hair Loss): You will lose hair on any part of your skin being treated, in most cases your whole body. This includes your head, eyebrows, pubic hair, hair on legs/arms, etc. Your hair will often grow back a few months after treatment ends. Wearing a hat and sunglasses can protect your scalp and eyes.
- Nail loss: Your finger and toenails will likely fall off. Keep your nails trimmed to avoid snagging or tearing them off. Keep your nail beds clean if the nails fall off. Do not use fake or acrylic nails.
- Fatigue: Fatigue is feeling very tired or exhausted. This is very common and tends to begin a few weeks into treatment. Fatigue often gets better slowly over the weeks and months after treatment.
- Loss of appetite: Loss of appetite is when you do not feel hungry, or you have no desire or interest in eating.
- Edema (swelling): Edema is the buildup of fluid within the body tissues and causes swelling or stiffness in the hands, legs/feet, and other joints.
Long-Term Side Effect
The most common long-term side effect of TSEBT is:
- Sweat Gland Changes: TSEBT can cause your sweat glands to not work as well after treatment. Sweating is one way your body cools off when it is hot. If you cannot sweat, you are at risk of overheating. To avoid this, stay out of the sun. When it is very hot outside, stay in the air conditioning when you can. Do not take part in activities that involve hot temperatures, such as saunas, steam rooms, hot tubs, and hot yoga classes.
There are ways to treat many of these side effects, including medications and therapy. After treatment, talk with your oncology team about receiving a survivorship care plan, which can help you manage the transition to survivorship and learn about life after cancer. You can make your own survivorship care plan using the OncoLife Survivorship Care Plan.