Anal Cancer: Staging and Treatment
What is staging for cancer?
Staging is the process of learning how much cancer is in your body, where it is, and if it has spread. Tests like digital rectal exams, biopsies using an anoscope, CTs and MRIs are done to help stage anal cancer. Your providers need to know about your cancer and your health so that they can plan the best treatment for you.
How is anal cancer staged?
Staging of anal cancer is based on:
- The size of your tumor.
- If the cancer has spread to the lymph nodes, and if it has, how many lymph nodes are affected.
- If the cancer has spread to other organs. This is called metastasis.
The staging system for anal cancer is called the “TNM system,” as described by the American Joint Committee on Cancer. It has three parts:
- T-Describes the size/location/extent of the "primary" tumor in the anus.
- N-Describes if the cancer has spread to the lymph nodes.
- M-Describes if the cancer has spread to other organs (metastases).
Your healthcare provider will use the results of the tests you had to determine your TNM result and combine these to get a stage from I (one) to IV (four).
Staging is important because it helps to guide your treatment plan. The staging system is very complex. Below is a summary of the staging system. Talk to your provider about the stage of your cancer.
- Stage I (1): The tumor is located in the anus and is 2 cm (centimeters) or less in size. It has not spread to the lymph nodes or to other organs.
- Stage IIA (2A): The tumor is located in the anus and is 2-5 cm in size. It has not spread to the lymph nodes or to other organs.
- Stage IIB (2B): The tumor is 5 cm or less in size and it has spread to the lymph nodes near the rectum, but has not spread to other body parts.
- Stage IIIA (3A): The tumor is larger than 5 cm in size and it has not spread to the lymph nodes or other body parts. OR, it is larger than 5 cm in size and it has spread to the lymph nodes near the rectum, but not to any other body parts,
- Stage IIIB (3B): The tumor is any size and is growing into nearby organs like the vagina, prostate gland, urethra, or bladder. It has not spread to the lymph nodes near the rectum, but not to other body parts.
- Stage IIIC (3C): The tumor is any size and is growing into nearby organs like the vagina, prostate gland, urethra, or bladder, AND it has spread to the lymph nodes near the rectum, but not to any other body parts.
- Stage IV (4): The tumor can be any size and may have spread to the lymph nodes and other body parts.
How is anal cancer treated?
Treatment for anal cancer is based on your health, your goals, the size of the tumor, and if it has spread to the lymph nodes or other organs. There can be more than one type of treatment used to treat anal cancer. Some of the treatments used are:
- Radiation.
- Chemotherapy.
- Surgery.
- Clinical Trials.
Often, chemotherapy and radiation are used together to treat anal cancer. This is called chemoradiation.
Radiation
Radiation is the use of high-energy x-rays to kill cancer cells. Radiation may be the only treatment for earlier-stage anal cancers or used in combination with chemotherapy. (chemoradiotherapy).
- You will get radiation treatment 5 days a week, and your healthcare team will tell you how many weeks you will get treatment.
- The treatments are painless and take just a few minutes.
- Radiation can irritate your skin causing it to become red, painful, or to break down. You may also experience have fatigue, diarrhea, and lower blood counts.
- Radiation to the pelvic area can impact sexual health and fertility. Before starting this treatment, be sure to talk with your provider about your sexual health and fertility.
Chemotherapy
Chemotherapy is the use of anti-cancer medicines that go through your whole body. These medicines may be given through a vein (IV, intravenously) or by mouth. Chemotherapy in anal cancer can be used with radiation therapy or as the only treatment, depending on the stage of your cancer.
The chemotherapy medications used to treat anal cancer include 5-FU, mitomycin, capecitabine, cisplatin, paclitaxel, oxaliplatin, leucovorin, and docetaxel. These may be used in combination and you may be given more than one medication, which is called a regimen.
Two newer medications, nivolumab and pembrolizumab, are also being used to treat anal cancer. These medications are called monoclonal antibodies. They work to stimulate the immune system to destroy cancer cells. These may be used in patients with metastatic disease or those whose cancer has progressed after their first treatments.
Surgery
Surgery is not often used to treat anal cancer. It may be used in an early stage, superficial cancer, also called perianal cancer. The surgery to remove the tumor is called a local excision.
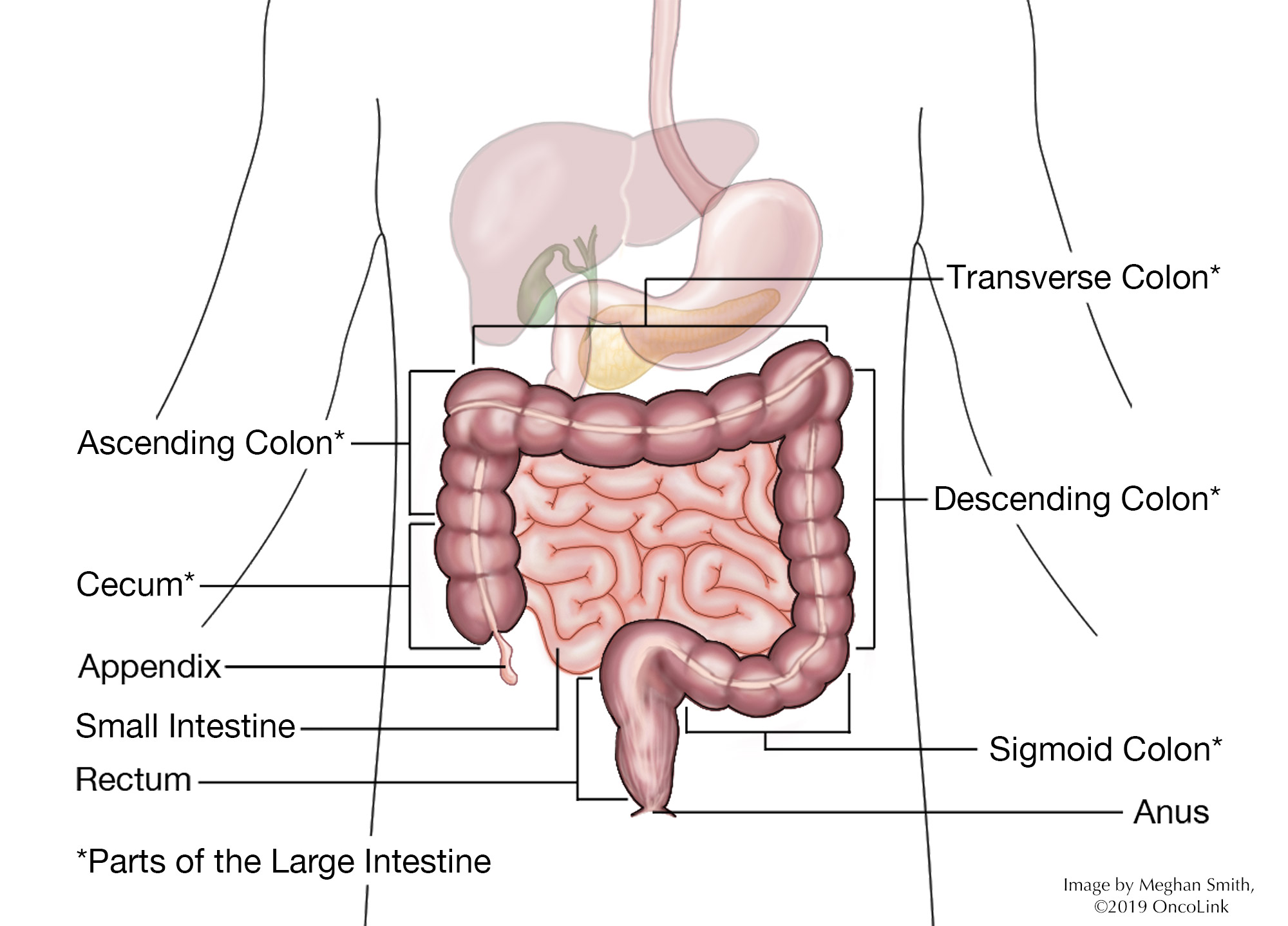
If you have advanced anal cancer or cancer that has come back after treatment or has not responded to treatment, your provider may recommend an abdominal perineal resection (APR). In this surgery, the anus is cut, including the anal muscles, and a permanent colostomy to collect stool is placed.
Clinical Trials
You may be offered a clinical trial as part of your treatment plan. To find out more about current clinical trials, visit the OncoLink Clinical Trials Matching Service.
Making Treatment Decisions
Your care team will make sure you are part of choosing your treatment plan. This can be overwhelming as you may be given a few options to choose from. It feels like an emergency, but you can take a few weeks to meet with different providers and think about your options and what is best for you. This is a personal decision. Friends and family can help you talk through the options and the pros and cons of each, but they cannot make the decision for you. You need to be comfortable with your decision – this will help you move on to the next steps. If you ever have any questions or concerns, be sure to call your team.
You can learn more about anal cancer at OncoLink.org.