Understanding Your Pathology Report: Colon Cancer
What is a pathology report?
A pathologist is a doctor who specializes in diagnosing diseases by looking at tissue from your body. The pathologist writes a report of their findings. This is called the pathology report. This report has important information about your tumor and helps guide your treatment plan. You should request a copy of this report and keep it in your files.
You will probably never meet the pathologist, but samples of your colon tissue that are removed during surgery or biopsy will be sent to them for review.
What will you find in a pathology report?
Pathology reports may differ depending on which lab and doctor write them. In general, the report contains:
- Demographic information: Name, birth date, medical record number, presumed diagnosis (if known), and your doctor’s name.
- Description of the procedure and how/where the sample was taken.
- Gross description: This describes what the pathologist saw without a microscope or other tools. The pathologist may describe the color, weight, and size of the tissue.
- Microscopic description: What the sample looks like under the microscope.
- Tumor cell type: Describes the type of cells that make up the tumor. Adenocarcinoma is the most common type of colon cancer.
- Histologic grade: How different the cells look compared to normal cells.
- Lymphovascular Invasion: Describes if the cancer cells have gotten into the lymph or blood systems.
- T-stage: Describes the tumor size and how far it is growing into the wall of the colon.
- Lymph nodes: How many lymph nodes were tested, and how many have cancer cells in them.
- Margins: The pathologist looks at the edges of the sample to be sure there are no cancer cells near the edge or beyond.
- Diagnosis: Based on all the information above, the pathologist gives a diagnosis.
To help you better understand your report, let's go through these sections one at a time.
The Gross Description
This is a description of the sample that the pathologist received and what they see without a microscope or other tools. In a biopsy, the sample that the pathologist looks at is likely a small piece of tissue and may describe the color, shape, feeling, and size of the tissue. After a cancer surgery, some organs or tissues may be sent to the pathologist and described in the report. This might include size, color, and weight. For example, a colon sample from a colectomy may be described as:
"Sample #1 is labeled ‘colon’ and consists of a segment of bowel measuring 13 cm in length after fixation. The sample is surrounded by a moderate amount of pericolonic fat. 3 cm from one resection margin is an ulcerated round tumor measuring 3.2 cm in diameter. The rest of the mucosa is grossly unremarkable."
This tells us the sample was a 13 cm long piece of the colon, with a tumor found 3 cm from one end.
Microscopic Description
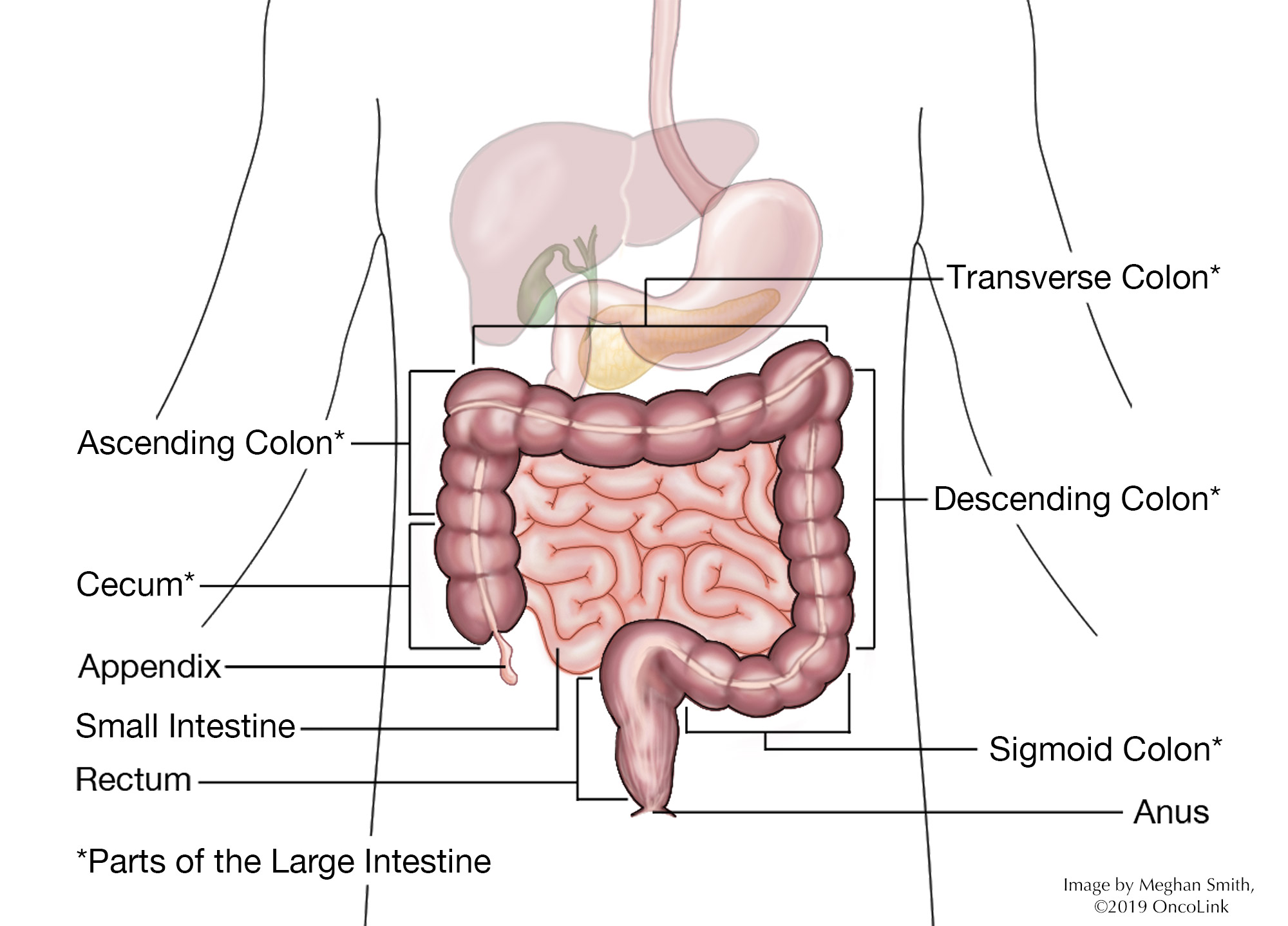
We need to know more about the colon to understand this part. The colon, or large intestine, is a tube that is about 5 to 6 feet in length. The first 5 feet make up the colon, which then connects to about 6 inches of the rectum, and ends with the anus.
The colon is made up of several sections. Your report may state which section the tumor was in. These sections are called the cecum, the ascending, transverse, descending and sigmoid colons, the rectum, and the anus (see diagram). The splenic and hepatic flexures are where the colon bends (or flexes) and are named for the organs they are near.
The colon is shaped like a tube and is made up of many layers. The layers start with the innermost layer called the mucosa (made up of epithelium), and then the lamina propria and muscularis mucosa. This is surrounded by the submucosa, which is surrounded by two layers of muscle (or muscularis). Lastly is the serosa layer, which is the outside layer of the tube. The outside of the colon is covered with a layer of fat, called adipose tissue, that has lymph nodes and blood vessels that feed the colon tissue.
Tumor Cell Type
The type of colon tumor describes which type of cells the tumor comes from. There are many different types of colon tumors:
- Adenocarcinoma is the most common type, making up more than 95 out of 100 cases of colon cancers. An adenocarcinoma comes from the glandular cells that line the inside of the colon. Two subtypes of adenocarcinoma are signet ring and mucinous, which are both named for the way the cells look under the microscope.
The following tumor types make up between 2 and 5 out of 100 cases of cancers found in the colon. These tumor types are not discussed in this article:
Polyps
A colon polyp is a benign (noncancerous) growth. Over time, polyps can turn into cancer. For that reason, they are removed during a colonoscopy and may be sent to the pathologist to decide what type of polyp it is. Several types of polyps can be found in the colon:
- Tubular adenoma (also called adenomatous polyp): Makes up 70 out of 100 cases of polyps found in the colon and can progress into cancer, but this happens over many years. If they are found early, they can be removed during a colonoscopy.
- Villous adenoma: Makes up 15 out of 100 cases of polyps found in the colon. This type of polyp has the highest risk of turning into cancer. In some cases, these can be removed during a colonoscopy. Sometimes surgery is needed to remove this type of polyp.
- Hyperplastic polyps and Inflammatory (or pseudopolyps): These two types of polyps are not likely to turn into cancer.
Colon polyps come in two forms:
- Pedunculated: These grow on a stalk and look like a small mushroom, which can often be seen and removed during a colonoscopy.
- Sessile: These are flat and grow on the wall of the colon. These can be harder to remove and may need surgery to remove the entire polyp.
Histologic Grade
As normal cells develop, they "differentiate" to become a certain type of cell. Histologic grade describes how closely the tumor cells look like normal cells. The more a tumor cell looks like a normal cell, the more well-differentiated it is. On the other hand, the more cells do not look like normal cells (higher grade), the more aggressive they are. They can grow and spread faster. Histologic tumor grade is broken down as follows:
Tumor Grade (G)
- GX: The tumor grade cannot be identified.
- G1: Well differentiated. Cells look the most normal.
- G2: Moderately differentiated. Cells look somewhat like normal cells.
- G3: Poorly differentiated. Cells look less like normal cells.
- G4: Undifferentiated. Cells look the most abnormal and barely look like normal cells.
Lymphovascular Invasion
When the pathologist looks at the sample of the tumor and nearby tissue, they look at the tiny blood vessels and lymphatic drainage to see if any tumor cells have grown into them. This is called lymphovascular invasion. This may be a sign of a more aggressive or advanced tumor. This is not the same as cancer cells that are found in the lymph nodes.
T Stage/Depth of Invasion
A tumor that has not grown into the surrounding tissues is sometimes called "in situ,” while tumors that have grown into nearby tissues are called invasive. T stage is classified as:
- Tx: The tumor cannot be measured.
- T0: There is no evidence of a tumor.
- T1s: The cancer cells are found only in superficial (close to the surface) tissue, often called cancer in situ or pre-cancer.
- T1, T2, T3, or T4: Describes the tumor based on size and if it has spread to nearby tissues and structures.
Some examples are:
- "The biopsy shows involvement of the mucosal lamina propria by neoplastic glands. The submucosa is not involved." This tumor invades only the innermost layer of the colon (T1s).
- "The tumor invades through the muscularis propria but not into the pericolonic adipose tissue. The serosal surface is not involved." This tumor invades the muscle layer but does not invade the serosa (the outer layer of the colon) or the surrounding fat (T2).
- "The tumor is invasive through the muscularis propria into the pericolonic fat." This tumor has penetrated through the colon wall and into the surrounding fat (T3).
Lymph Nodes
The lymph system is often called the "housekeeping system" of the body. It is a network of vessels (tubes) that connect the lymph nodes. These nodes have cells that clear bacteria and other foreign debris from the body. Lymph is a watery liquid that flows between cells in the body, picking up debris and taking it into the lymph node for filtering and then to the liver, where it exits the body.
Cancer cells use the lymph system as a first step to traveling to other areas of the body. During colon cancer surgery, many lymph nodes are removed and checked to see if there are cancer cells in them. This will be stated in the report as the number of lymph nodes that had cancer cells and how many were checked. For example, the report might state "fifteen benign lymph nodes (0/15)" or "tumor seen in sixteen of twenty lymph nodes (16/20)."
It is not uncommon to have as many as 30 lymph nodes removed during a colon cancer surgery. This is different from many other types of cancer, where far fewer nodes are removed.
Margins
This is the area at the edge of the sample that the pathologist looks at. During surgery for cancer, the surgeon tries to remove the whole tumor and some normal tissue surrounding it. This area of "normal tissue" is important because any stray cancer cells may be included in this. If the edge (or margin) contains tumor, there may have been cancer cells left behind. The goal of surgery is to achieve a "clear margin,” that is, clear of any cancer cells.
Putting it All Together
All of these pieces are used to figure out the stage of the cancer and what treatment is needed. By understanding the basics of the report, you will be able to talk about your treatment options with your healthcare team. You can learn more about colon cancer staging and treatment here.
Molecular Markers
A molecular marker is something found in the blood, tissue, or other body fluid that is a sign of a normal or abnormal process, condition, or disease. Some tumors have markers that can give an idea of the risk of the cancer coming back after treatment (prognostic marker) or predict response to cancer treatment (predictive marker). Two molecular markers found in colon cancers are "microsatellite instability" and "18q loss of heterozygosity."
- Microsatellite Instability: Microsatellite DNA is made up of nucleotide sequences, repeated over and over and linked together. It is found in all human genes. Molecular testing can find instability or mistakes in the microsatellite DNA of tumors. One type of change is the number of repeat sequences. This is called microsatellite instability (MSI). MSI is a way to measure a deficiency of mismatch repair (MMR) in tumor DNA. A deficiency of MMR causes more mutations within colon cells. This may raise the risk of colon cancer. MSI testing identifies tumors as MSI-H (i.e. MSI-high), meaning they lack MMR proteins or are deficient in MMR proteins (dMMR), or MSI-stable and MSI-low, meaning they are considered MMR proficient (pMMR) or have most or all of the MMR proteins.
There are two reasons to test colorectal cancers for MSI:
- To find those at risk for hereditary non-polyposis colon cancer (HNPCC). People with HNPCC may be at a higher risk for other cancers, including endometrial, stomach, ovarian, pancreatic, and kidney cancers. If you have HNPCC, talk with your care team about genetic testing, cancer screenings, and prevention based on family history and personal risk.
- In early-stage colon cancers, MSI may affect treatment options. About 22 out of 100 cases of stage II (2) colon tumors have MSI-H. About 12 out of 100 cases of stage III (3) colon tumors have MSI-H. Many studies have found that patients with stage II MSI-H tumors did not get any benefit from 5-FU adjuvant therapy. MSI-stable disease, however, may benefit from 5-FU-based treatment. Some experts recommend MSI testing as another tool to figure out the need for treatment in stage II disease.
Other Markers
Humans have 23 pairs of chromosomes, for a total of 46 chromosomes, found in each cell in the body. Each chromosome has over 1000 genes. Over your lifetime, you can damage genes or chromosomes due to exposures, such as smoking and viruses.
Other molecular markers being studied include chromosome 18q, KRAS, BRAF, a tumor suppressor called guanylyl cyclase 2, p53, and ERCC-1. Studies have found some of these markers help pick the best treatment. For instance, anti-cancer medications that target the EGFR protein, such as cetuximab and panitumumab, will not be effective in people who have a KRAS or BRAF gene mutation (defect). These tests are not the standard at this time, but some providers are using them, so you may hear about them at your provider’s visits.
Talk to your provider about molecular marker testing and if it is right for you.
Resources for More Information
Oncolink: Stage II Colon Cancer: To Treat or Not To Treat?
American Cancer Society: Understanding your Pathology Report: Invasive Adenocarcinoma of the Colon: https://www.cancer.org/treatment/understanding-your-diagnosis/tests/understanding-your-pathology-report/colon-pathology/invasive-adenocarcinoma-of-the-colon.html