Barrett's Esophagus: An Overview
What is the esophagus?
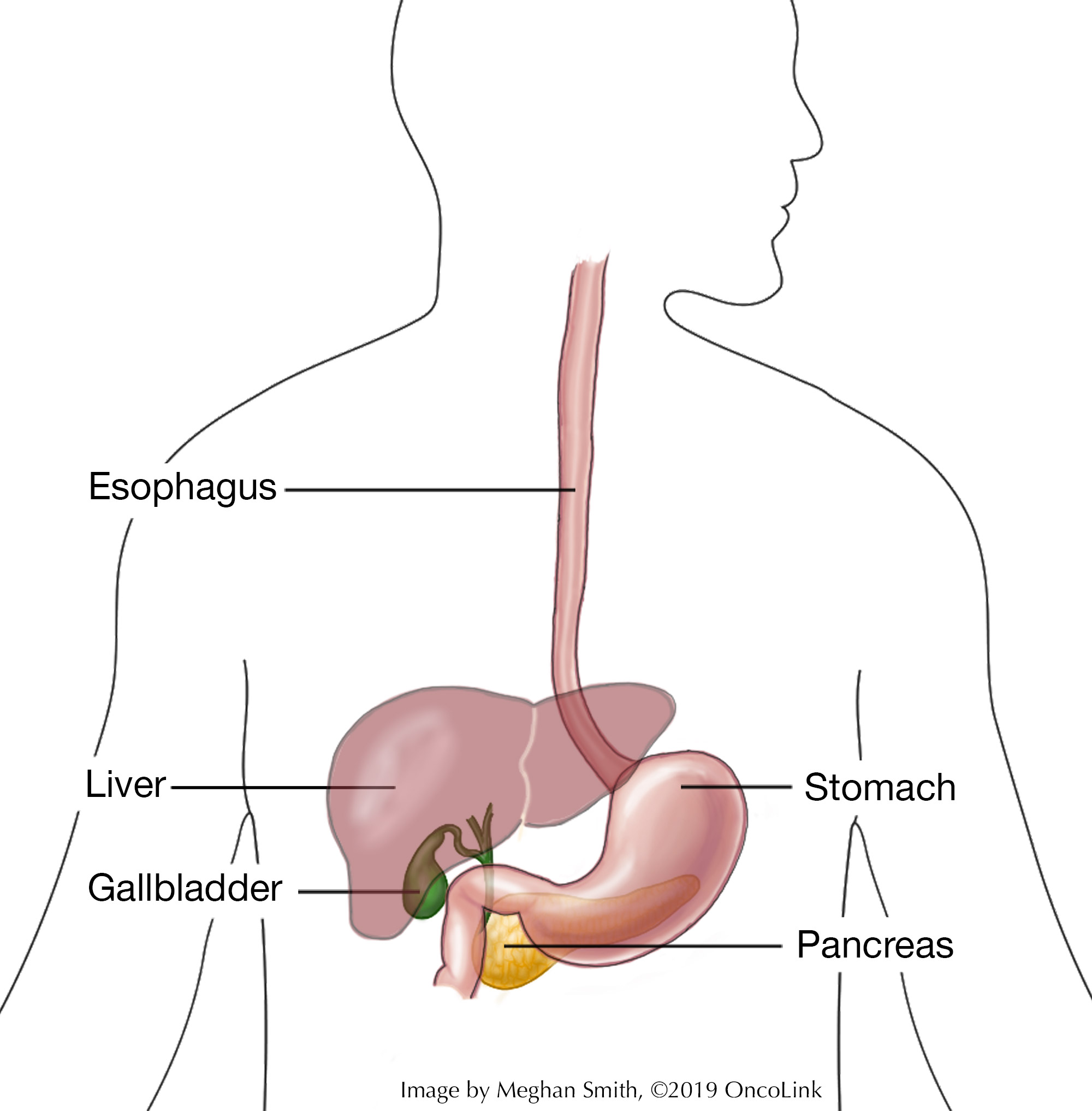
The esophagus is a muscular tube that connects the mouth to the stomach.
How does the esophagus work?
It moves the food we swallow from our mouths to our stomachs, where it can be digested. The esophagus is usually about 25 cm (10 inches) long and meets the stomach at the gastroesophageal junction (GE junction). At the GE junction, there is a circular muscle that wraps around the esophagus called the lower esophageal sphincter. This is not a muscle that we can control on our own. Normally, it opens only to let food from the esophagus into the stomach or during vomiting. The lower esophageal sphincter muscle stops food and stomach acid from coming back up into the esophagus.
The lining of the esophagus is called the mucosa, which protects the esophagus from things that might cause damage, like stomach acid. The cells that make up the mucosa are replaced at a fast rate to help fix the damage that happens during everyday eating. The cells in the mucosa are flat cells that have layers (called "stratified squamous epithelium").
What is stomach acid?
Stomach acid helps you digest food. But, it can cause damage if you have too much of it or if it comes back up into the esophagus.
What is Barrett's esophagus?
Barrett's esophagus happens when the cells that make up the lining of the esophagus change because of damage, and do not grow back normally. This change, called metaplasia, puts a person at higher risk of cancer. Instead of being made up of flat cells in many layers ("stratified squamous epithelium"), there is a single layer of tall-shaped cells ("columnar epithelium"), which can be pre-cancerous.
How is Barrett's esophagus related to esophageal cancer?
People with Barrett's esophagus have a higher risk of cancer of the esophagus than people who do not have Barrett’s esophagus. Barrett's esophagus increases the risk of a cancer called esophageal adenocarcinoma. Barrett's esophagus is a "premalignant" disease, meaning that while it is not cancer, it can become cancer.
Though the overall risk of esophageal adenocarcinoma is low, Barrett's esophagus is still very important clinically. This is because treatments for Barrett's are more successful than treatments for esophageal cancer.
What causes Barrett's esophagus and am I at risk?
The most common cause of Barrett's esophagus is gastroesophageal reflux disease (GERD), or heartburn. When a person has GERD, acid from the stomach splashes up into the esophagus causing repeated damage to the lining of the esophagus. Many people with Barrett's esophagus have a history of heartburn or acid regurgitation lasting at least 10 years. Some people, however, develop Barrett's esophagus without ever having any reflux symptoms. Some of the well-known risk factors are:
- Being 50 years old or older.
- Current or family history of Barrett’s esophagus.
- Male as the sex at birth.
- White (Caucasian) race.
- Having chronic GERD.
- Hiatal hernia (a condition where part of the stomach protrudes into the chest).
- Obesity.
Though less common and less well-studied, bulimia with vomiting can also increase the risk of Barrett's esophagus due to damage to the esophagus from repeated vomiting.
How can I prevent Barrett’s esophagus?
Ways to prevent Barrett’s esophagus focus on treating chronic GERD. Work with your provider to make a plan. This plan might include:
- Taking antacid medications.
- Stopping use of tobacco products.
- Managing weight.
- Eating small, frequent meals.
- Avoiding eating three hours before going to bed.
- Avoiding bending over after eating.
- Raising the head of your bed to help with digestion.
- Avoiding foods that are spicy, high-fat, dairy, or acidic.
What screening tests are available?
The American Gastroenterological Association does not recommend screening the general population for Barrett's esophagus. You should be screened if you have chronic and/or frequent symptoms of GERD and two or more risk factors for Barrett’s esophagus or esophageal adenocarcinoma. Women have a lower risk than men of getting Barrett’s esophagus. But, screening could be recommended for women who have risk factors. The risk factors are the same for women and men.
There is a lack of evidence to guide screening, and the screening is invasive and expensive. Before any screening is done, the current health and life expectancy of a patient should be considered. Screening for Barrett’s esophagus can be done in two ways:
- Upper endoscopy: In this procedure, you are sedated and a camera on a long, thin tube is put into your mouth, and down your throat so your provider can see into your esophagus.
- Unsedated transnasal endoscopy: In this procedure, a long, thin tube is put into your nose and down your throat to see your esophagus.
What are the signs of Barrett’s esophagus?
Signs of GERD can also be signs of Barrett’s esophagus. Signs of both are heartburn, belching, nausea, regurgitation, bitter taste in the mouth, abdominal discomfort, and dry cough.
How is Barrett's esophagus diagnosed?
Barrett's esophagus is diagnosed by upper endoscopy. Upper endoscopy lets your provider look at the insides of these organs and find ulcers, abnormal growths, and other conditions like Barrett's esophagus. During endoscopy, many biopsies are taken. The tissue is then looked at under a microscope to see if there are changes in the cells of the mucosa that look like Barrett’s esophagus. Biopsies are also important to make sure that there is no cancer present. All biopsies should be examined by two or more pathologists, and at least one should be an expert in esophagus pathology.
How is Barrett’s esophagus staged?
The severity of Barrett's esophagus is described in two ways:
- If there is dysplasia and the degree.
- The amount of disease (measured by the Prague Criteria).
Dysplasia describes an abnormal appearance of cells under a microscope. More highly abnormal cells are more likely to become cancer. Dysplasia can be either low-grade or high-grade, and exists on the following spectrum:
- Metaplasia
- Low-grade dysplasia.
- High-grade dysplasia.
- Invasive cancer.
The Prague C&M Criteria are a set of rules that allow your care team to find out how severe Barrett's esophagus is. The criteria is described here:
- The "C" is the Circumferential extent of disease. It is determined by measuring the distance from the GE junction to the highest area where metaplasia is around the circumference of the esophagus.
- The "M" is the Maximum extent of disease. It is the distance from the GE junction to the highest area of metaplasia.
The higher the Prague C&M numbers (eg. C3 M5), the more severe the Barrett's esophagus and the higher the risk of cancer.
How is Barrett's esophagus treated?
Treatment in people with Barrett's esophagus is aimed at treating acid reflux. This is often done by using medications. However, surgery and methods of endoscopic eradication can also be used.
Medication
Some medications may be prescribed, such as proton pump inhibitors (omeprazole, lansoprazole, pantoprazole, etc) and H2-blockers (famotidine). These medications work by lowering the amount of acid that is made in the stomach. Proton pump inhibitors are often more effective than H2-blockers. In recent years, it has been researched whether aspirin can lower the risk of esophageal adenocarcinoma. At this time, aspirin and non-steroidal medications should not be routinely prescribed to patients with Barrett’s esophagus unless indicated as treatment for another medical condition.
Surgery
There are also many anti-reflux surgeries, such as fundoplication, that can be done to control reflux. The American College of Gastroenterology does not recommend anti-reflux surgery or high-dose proton pump inhibitors for the prevention of adenocarcinoma of the esophagus – though these therapies can and should still be used to treat symptoms of chronic reflux.
In some cases, an esophagectomy may be done which removes part or all of your esophagus. Your esophagus is then rebuilt using parts of your stomach or large intestine.
Endoscopic Eradication
Endoscopic eradication (also called endoscopic ablation) is the attempt to remove abnormal cells and save as much of the normal esophagus. This surgery type uses the same techniques that are done during endoscopy. Endoscopic eradication is recommended for patients with high-grade dysplasia to try to get rid of all abnormal areas of mucosa. Patients with low-grade dysplasia may also be treated with endoscopic eradication, but may also be followed only with endoscopic surveillance (a set schedule of endoscopies to keep an eye on abnormal cells). Often, Barrett’s esophagus may come back after eradication therapy. Your provider will continue to monitor you using endoscopy per their recommended schedule. There are many types of endoscopic eradication:
- Radiofrequency ablation uses electricity and heat to damage cells and is aimed at abnormal areas.
- Photodynamic therapy uses a chemical called a photosensitizer and a light source. The photosensitizer is put on tissues or areas the clinician wants to eradicate; when light is directed at those cells, the reaction between light and the photosensitizer causes cell death.
- Cryotherapy uses extreme cold to get rid of damaged cells.
- Endoscopic mucosal resection is a procedure where part of the lining of the esophagus is surgically removed and is recommended if your care team thinks you have cancer.
Patients who get eradication therapy will go to a center that specializes in the treatment of esophageal and stomach cancer. This center will be able to do surgery or remove the esophagus if needed.
Clinical Trials
You may be offered a clinical trial as part of your treatment plan. To find out more about current clinical trials, visit the OncoLink Clinical Trials Matching Service.
Follow-Up Care
Although it is not common for Barrett’s esophagus to lead to esophageal cancer, there is still a risk so it is important to follow your provider’s suggestions for treatment and follow-up care. Make sure to follow screening guidelines and the schedule you are given for imaging if you are at risk for developing esophageal cancer.
This article serves as an introduction to Barrett's esophagus. More information about esophageal cancer and its treatment can be found at OncoLink. You should talk to your provider if you are concerned about Barrett's esophagus or esophageal cancer.