Intracavitary Brachytherapy for Gynecologic Cancers – Vaginal Cylinder
What is brachytherapy?
Brachytherapy is the use of radiation that is put inside your body. This allows a higher dose of radiation to directly reach the area where the tumor is or was before surgery. In the case of brachytherapy for gynecological cancers, it reduces radiation exposure to the surrounding healthy tissues, such as the bowel and bladder. Brachytherapy is given after the placement of an applicator. An applicator helps guide where the treatment will be given.
In the treatment of gynecological cancers, brachytherapy may be given in addition to traditional external beam radiation. How often you receive brachytherapy will be determined by your care team. Ask your provider what your schedule will look like before starting treatment.
What is a vaginal cylinder?
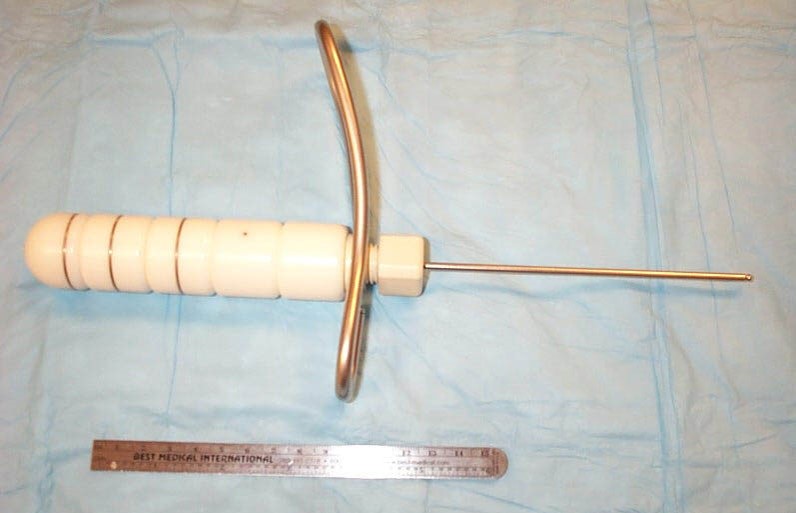
The radiation needs to be placed near your cancer or where your cancer was removed. To be able to do that, applicators are used. One type of applicator that can be used is a vaginal cylinder. This is often used in women who have had a hysterectomy. A vaginal cylinder is made of plastic and looks like a large tampon with a hollow center. It is placed into your vagina and may be kept in place with gauze, balloons, or a special undergarment.
How is the brachytherapy administered?
Before your brachytherapy treatment, the vaginal cylinder will be placed by your provider. You will be asked to lay down on a table and place your feet in stirrups as you would for a gynecologic exam. Your provider may do a short exam and then the cylinder will be placed in your vagina. You may feel pressure while the cylinder is being placed. If you are very uncomfortable, you should tell your provider. There are different sizes of cylinders, and you may need a smaller size. An x-ray may be done to check the placement of the cylinder.
Before Treatment
Before starting treatment, you will need to have a simulation or planning appointment. This may be done before starting treatment or on your first day of treatment. During this appointment, after the cylinder has been placed, your provider may place a “marker” (this may be a large-Q-tip soaked in contrast solution or a fiducial seed) into the top of your vagina. This will help guide where the radiation needs to go during the planning. You will have imaging studies done such as MRIs and CT scans.
After the imaging studies have been done, it can take your care team a few hours to plan your treatment. This is because they need to make sure the radiation is going to the correct spot. During this time, you may need to lay flat or with your head only slightly elevated.
During Treatment
Once your plan is ready, you will be asked to continue lying in the same position for treatment that you were in during your imaging tests. Positioning is very important in radiation therapy. Your body will be positioned carefully in order to get the best radiation treatment and you will be in the same position during every treatment. Once in position, the cylinder is connected to a machine that feeds the radiation source into the applicator, where it remains for a set amount of time, known as the dwell time. It is important to lie still during your whole treatment. Once the time is up, the machine removes the source and the applicator can be removed from your vagina. The radiation treatment time can vary.
Keep in mind that you will be by yourself in the room as the brachytherapy is being given. This is to protect the staff from the effects of the radiation. Make sure that you have no needs that have not been met before the therapy starts and that you are comfortable. You will be able to talk with the therapists the entire time and if you have any emergent needs you should tell them. The therapists will be monitoring you during treatment from the cameras in the room.
After Treatment
Once your treatment is done, a provider will remove the vaginal cylinder. The cylinder may be kept in place for minutes to days depending on your treatment plan. It is removed after each treatment and you will be able to go home shortly after your treatment is done.
What can I expect after the treatment?
Your provider should talk with you about what you can expect after treatment, these may include:
- Vaginal discharge after the applicator is removed. You can use a pad, but should not use tampons to manage the discharge. This can be pinkish in color and should not last for longer than a few days.
- Cramping, like menstrual cramps, for 24 hours after the procedure. You may use ibuprofen (Advil, Motrin, or Nuprin) or naproxen (Aleve or Naprosyn) to relieve the cramps. Be sure to follow the instructions on the bottle.
- Diarrhea. You can take over-the-counter medications, such as loperamide (Imodium) or Kaopectate, to help manage any diarrhea. See our managing diarrhea teaching sheet for other tips on managing diarrhea.
- Do not have sexual intercourse (or place anything into the vagina) during treatment and for a time after treatment. It could cause tenderness and irritation in your vagina.
- To be given vaginal dilators to use once your treatment is done. These will help your vaginal tissue remain flexible, making intercourse more pleasant, but also making pelvic exams more comfortable. You will need to use the dilator for the rest of your life. See our teaching sheet on dilators to learn more about them.
After treatment, you are not radioactive and it is safe for you to be around friends and family. You can eat a normal diet and carry on your normal activities unless your provider tells you otherwise.
When should I call my care team?
Reasons to call your care team:
- You develop a fever (temperature > 101).
- You have pain that is not relieved with over-the-counter medication.
- You have a lot of bleeding (more than a menstrual period) or develop vaginal discharge.
- You have burning or blood in the urine more than 24 hours after the procedure.
- You do not have a bowel movement for 3-4 days after the procedure.
- You have more than 3-4 episodes of liquid diarrhea a day.
Brachytherapy using a vaginal cylinder may be given differently at each cancer center. Ask your provider what you should know before starting treatment and ask any questions that you may have.