Jackson-Pratt (JP) Surgical Drain
During some types of surgery, your surgeon may need to place a drain under your skin. A drain helps bodily fluids leave your body so that they do not collect under or near your incision (surgical cut). Removing these fluids helps the wound heal, can prevent infection, and can lessen the amount of drainage on surgical bandages. There are a few kinds of surgical drains. One common type is called a Jackson-Pratt drain, or JP drain.
How does a JP drain work?
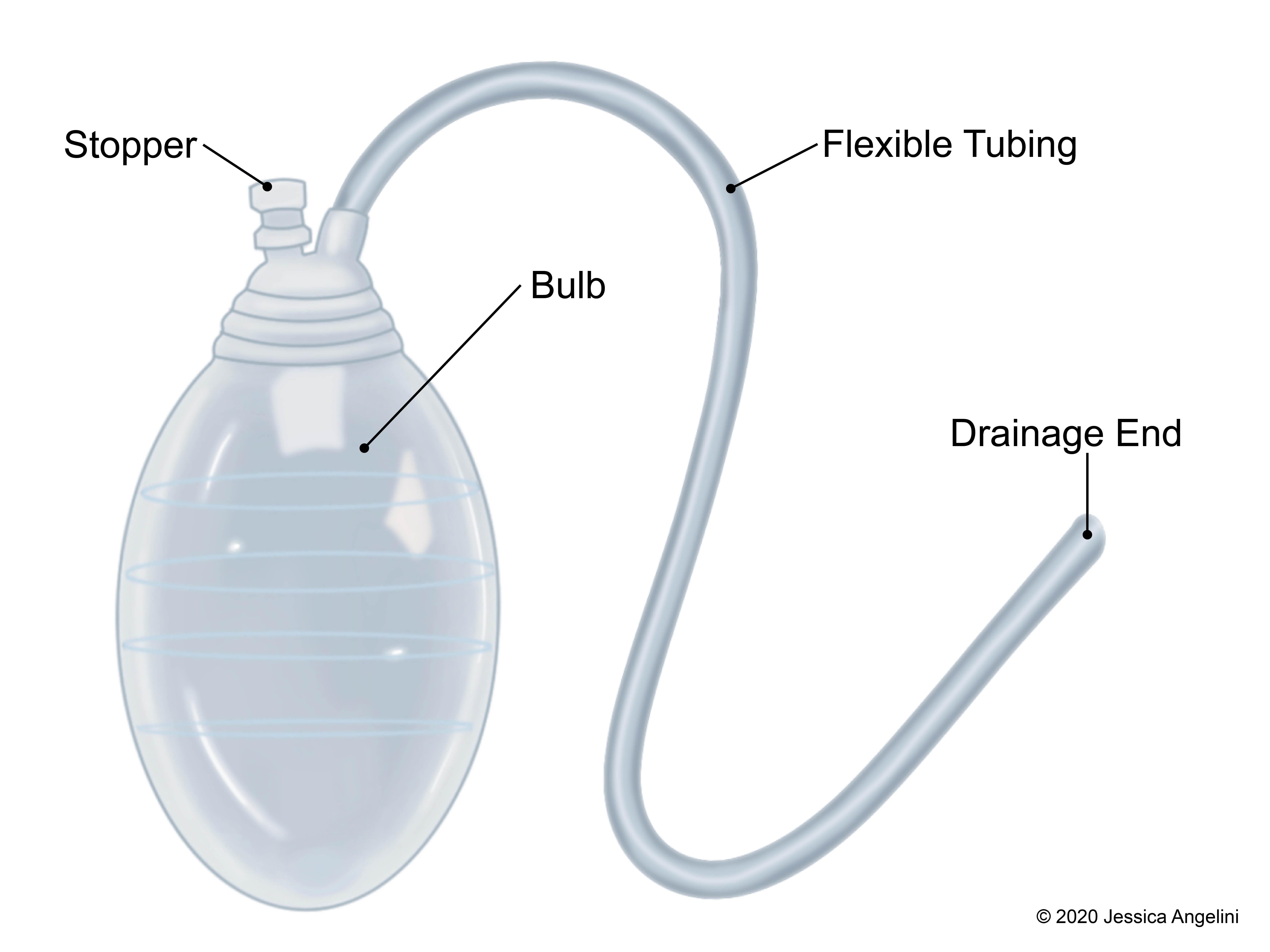
A JP drain is a closed suction device. This means that the fluids are collected within a closed system, without the need for an outside suction machine. A JP drain has a thin, flexible rubber tube that sits under the skin in the area under or near the incision. Often, your skin and the tube are sutured (stitched) together to make sure the JP drain does not move from under your skin. At the end of the tube is a small squeeze bulb. Bodily fluids pass through the tube into the bulb. The bulb has a plug, or stopper, where you can empty fluids and push air out.
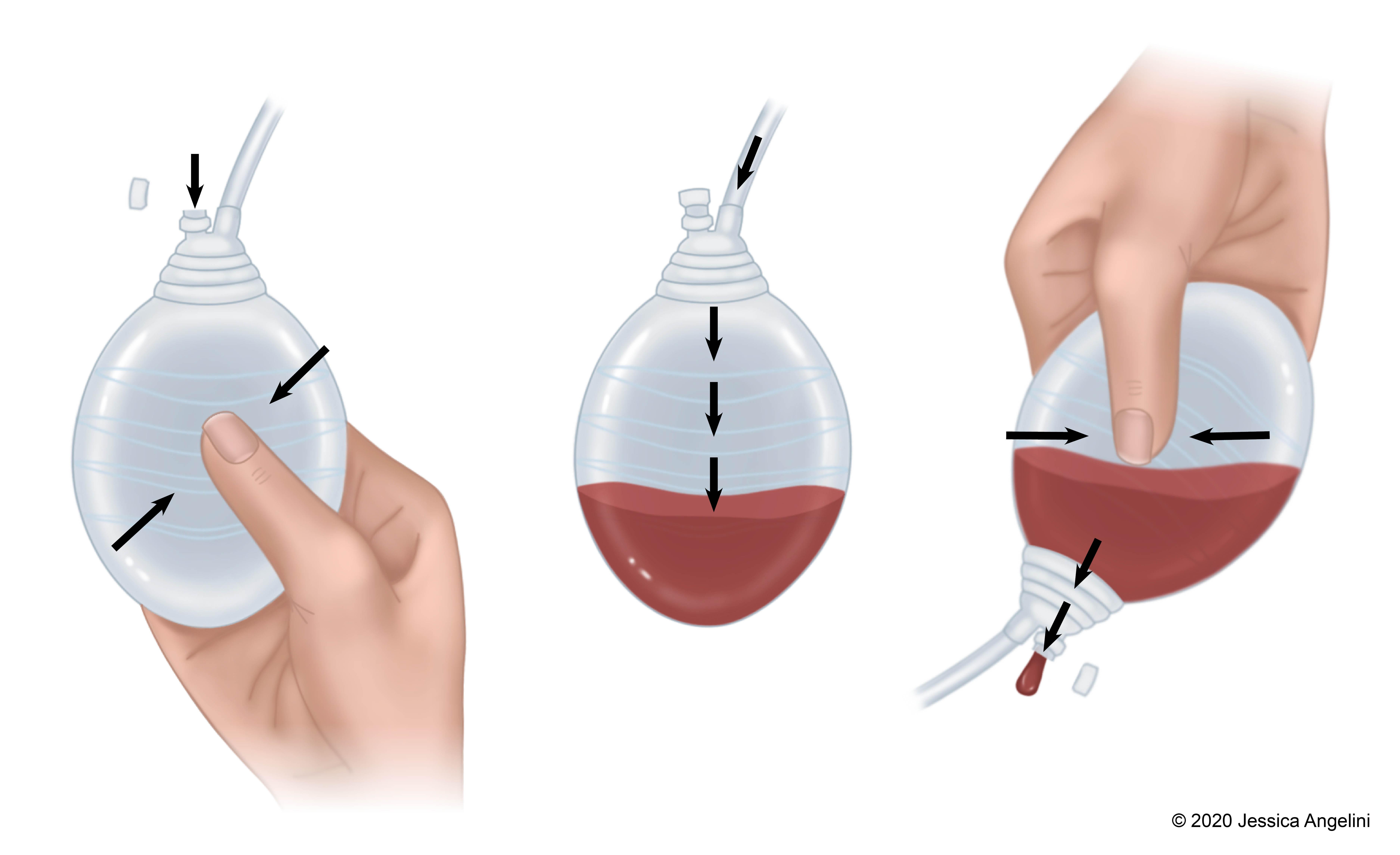
When air is removed from the bulb (done by squeezing it), it will start to suction. This suction, or “negative pressure,” will gently pull the fluids out from your body and into the bulb. The plug on the bulb is opened to drain the fluid that collects and then closed to start the suction again. It is important to squeeze the air out of the bulb each time you empty it so that the suction, or negative pressure, can keep pulling the fluid out of your body.
How do I care for my JP drain?
Your care team will teach you how to care for your wound and drain. Talk with your care team if you or your caretaker have any questions about caring for your drain. Some general tips for caring for your JP drain are:
- Always wash your hands before and after touching or emptying the drain.
- You will be given a measuring cup to measure the fluids that drain into the bulb. Keep all of your supplies together.
- Write down in a notebook the time and how much fluid you empty. The number of times you have to empty the drain depends on the type of surgery you had and what your care team taught you.
- Sometimes the fluid that goes into the tubing can have stringy pieces that block the tube from draining into the bulb. Your provider may teach you how to “strip” or “milk” the tubing. Stripping/milking the tube is a way to gently massage the tubing to clear any blockages. Ask your provider if and how you should do this.
- When you unplug the stopper on the bulb to empty the fluids, try not to touch the inside of the plug or bulb.
- Turn the bulb over to drain the fluids into the measuring cup. Keep squeezing until all the fluid is out and close the plug while the bulb is flat (with all of the air pushed out).
- Flush the fluids down the toilet or sink once you have measured them. Rinse the measuring cup out after you have emptied it.
- Don’t let the tubing and bulb dangle freely. To keep from pulling on the tubing, you may need a safety pin to attach it to your clothing, near where the tubing begins. Talk with your provider about where and how you should secure your drain so that it doesn’t pull.
- The color of fluid that drains will change as you heal from surgery. Often, it will start as a dark red color and become a pink or yellow color.
- Ask your provider how you should bathe or shower while the drain is in place.
- You may also be taught how to change the dressing where your JP drain was placed. If it becomes saturated (soaked with blood or fluid) or wet, you should change it.
When should I call my provider?
If you or a caretaker have any questions about caring for your drain while at home, call your provider. Some reasons you should call your care team right away are if:
- There is new or more leaking from the area around the tubing, where it enters your body.
- The tubing is pulled and comes out (this is rare since the tubing is stitched into your skin).
- The amount of drainage suddenly decreases or stops.
- The fluids that drain are cloudy or have a bad smell.
- The bulb won’t stay flat or decompressed.
- There is redness, swelling, pressure, or warmth where the tubing enters your body, or if you have a fever. Your provider will tell you at what temperature you should call them.
The length of time that you have the JP drain depends on the type of surgery you had and how much drainage you are having. When it is time for the drain to be removed, your provider will either remove it in the office or it will be removed by a home care nurse. This is quick and often painless. Your provider will then tell you how to care for your skin and what to look for once the drain is out.