Treatment for Lymphedema: Complete Decongestive Therapy
Treatment for Lymphedema: Complete Decongestive Therapy
Lymphedema happens when there is damage to your lymph nodes or lymph vessels. This can be caused by some treatments for cancer, including surgery and radiation. The main treatment for lymphedema is complete decongestive therapy (CDT). This can also be called complex decongestive therapy.
What is the Lymphatic System & Lymphedema?
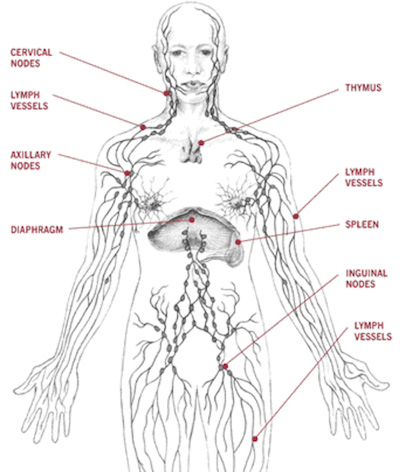
The lymphatic system is a group of lymph nodes and lymph vessels that run throughout your body. The lymph vessels run very close to your blood vessels and move fluid from the body through the lymph nodes and then into the blood.
Lymph nodes work as filters to fight infection and help regulate fluid.
- Lymph: A thin, clear fluid that circulates (moves) throughout your body. It removes wastes, bacteria, and other things from tissues
- Edema: The buildup of too much fluid.
Lymphedema happens when too much lymph collects in any area of your body. This buildup can be caused by a blockage in the system or damage to the lymph nodes or vessels. Fluid builds up in soft body tissues and causes swelling.
Lymphedema may be caused by the cancer, surgery, chemotherapy, or radiation. Surgery and radiation can cut off or damage some of the nodes and vessels that lymph moves through. Over time, the flow of lymph can be too much for the pathways that are still open and working, causing a backup of fluid into tissues.
Lymphedema causes chronic swelling that leads to scarring. The swollen body part feels harder to touch and is heavier than the non-swollen side. Lymphedema can cause increased limb size which can affect your mobility (how you move the limb) and can cause pain.
How is lymphedema treated?
Complete decongestive therapy (CDT) is used to treat lymphedema.
What is complete decongestive therapy (CDT)?
The goals of Complex Decongestive Therapy (CDT) are to:
- Lessen swelling.
- Improve skin condition.
- Increase mobility.
- Decrease discomfort.
- Lower your infection risk.
- Focus on your overall health and well-being.
Complete decongestive therapy (CDT) has many parts:
- Manual Lymphatic Drainage (MLD): A light skin stretching technique that stimulates (revs up) your lymphatic system. MLD uses light touch to move extra lymph and fluid out of the tissues and back into the lymphatic vessels.
- Compression/Bandages: Layered bandaging with foam or specially-fitted garments that support the affected area to control swelling. Wearing a compression sleeve or elastic bandage may help move and prevent the buildup of fluid.
- Exercises: With compression, special exercises will help pump lymph out of the swollen area.
- Skin Care: Keeping the skin clean and moisturized will help prevent infections that can happen with lymphedema.
- Self-Care Management: Learning how to manage your lymphedema on your own is a key part of your treatment. Studies suggest that to manage your symptoms, you should eat a healthy diet, control your body weight, and learn how to reduce injury to the area.
How long does treatment last?
How long treatment lasts depends on the patient. There are two phases of treatment:
Phase 1: Active Phase
The goal of Phase 1 is to get the extra lymph out of the affected body region, to lessen visible swelling, and to reduce other symptoms of lymphedema.
Phase I includes manual lymphatic draining (MLD), bandaging, exercises, skincare:
- The number of weeks depends on the amount of swelling, tissue firmness, and how long it takes for your symptoms affecting the skin to improve. On average, treatment lasts 2 to 4 weeks.
- Complete decongestive therapy for one-hour sessions, 4 to 5 days per week.
- Bandages with foam are worn about 23 hours per day and often only removed to bathe.
- Exercises are done to help encourage the drainage of lymph from affected tissue.
- Skin and nail care are important. It’s important to protect your skin in the affected area. Try to keep this skin from drying, cracking, becoming infected, and breaking down.
Phase 2: Maintenance Phase
The goal of Phase 2 is to maintain and maximize the achievements of Phase I, and to gain long-term control of your lymphedema.
The maintenance phase includes MLD, compression garments, exercises, and skincare:
- Phase II of CDT lasts for many years or even for the rest of your life.
- Elastic compression garments that fit like a second skin are worn during the day.
- Bandages with foam are often worn at night to decrease daytime swelling.
- Exercises are done while wearing compression.
- Self-manual lymphatic drainage for about 20 minutes per day may be also prescribed by your healthcare professional.
How can I begin complete decongestive therapy?
Ask your provider for a referral and prescription for CDT.
How do I find a certified therapist?
It is important to see a physical or occupational therapist that has passed a special training course to treat lymphedema. You will see the initials CLT, certified lymphedema therapist, behind their name. Therapists who have passed a national certification test have CLT-LANA behind their name.
If you need to find a qualified lymphedema therapist in your area, you can consult the National Lymphedema Network website using the NLN "find treatment" feature.
Next Article: Lymphedema and Exercise FAQs »
Resources for More Information
BreastCancer.org. Complete Decongestive Therapy (CDT).
National Cancer Institute. Lymphedema (PDQ®) – Patient Version.
Norton School of Lymphatic System https://www.nortonschool.com/about-lymphedema.html
National Lymphedema Network https://lymphnet.org/what-is-lymphedema
Next Article: Lymphedema and Exercise FAQs »