Ovarian Cancer: Staging and Treatment
What is staging for cancer?
Staging is the process of learning how much cancer is in your body and where it is. For ovarian cancer, tests like ultrasound, biopsy, colonoscopy, X-Ray, CT scan, MRI, and bone scan may be used to help stage your cancer. Blood tests, like a complete blood count (CBC) and tumor marker tests (such as CA-125) may also be done to help stage your cancer. Your providers need to know about your cancer and your health history so that they can plan the best treatment for you.
Staging looks at the size of the tumor, where it is, and if it has spread to other organs. There are two staging systems used for ovarian cancer. The first system is called the FIGO (International Federation of Gynecology and Obstetrics) system. The second system is called the “TNM system,” as described by the American Joint Committee on Cancer. Both systems stage ovarian cancer based on 3 factors:
- T-describes the size/location/extent of the "primary" tumor in the ovaries.
- N-describes if the cancer has spread to the lymph nodes.
- M-describes if the cancer has spread to other organs (metastases).
Your provider will use the results of the tests you had to determine your FIGO and TNM result and combine these to get a stage from 0 to IV.
How is ovarian cancer staged?
Staging of ovarian cancer is based on:
- The size of your tumor.
- If the cancer has spread to the lymph nodes, and if it has, how many lymph nodes are affected?
- If the cancer has spread to other organs. This is called metastasis.
Staging may be done at different times during your treatment.
Ovarian cancer is staged using two systems. Both the FIGO and TNM system are used. Staging is based on:
- If the cancer has spread, and if so, how far.
- How much cancer is in your body.
The staging systems are very complex. Below is a summary. Talk to your provider about the stage of your cancer.
AJCC and FIGO Stage I:
- Cancer is only in the ovary/ovaries. It has not spread to nearby lymph nodes or to distant sites.
AJCC and FIGO Stage IA:
- Cancer is in one ovary and only inside the ovary. It is not on the outside of the ovary or in any fluid or washings from the abdomen (belly) and pelvis. It has not spread to nearby lymph nodes or to distant sites.
AJCC and FIGO Stage IB:
- Cancer is in both ovaries, but not on the outside of either ovary or in any fluid or washings from the abdomen or pelvis. It has not spread to nearby lymph nodes or to distant sites.
AJCC and FIGO Stage IC:
- The cancer is in one or both ovaries and any of the following:
- IC1: The tissue around the tumor broke during surgery, which could lead to cells leaking into the abdomen and pelvis.
- IC2: Cancer is on the outer surface of one or both ovaries, or the capsule burst before surgery.
- IC3: Cancer cells are found in the fluid or washing from the abdomen and pelvis.
- It has not spread to nearby lymph nodes or to distant sites.
AJCC and FIGO Stage II:
- The cancer is in one or both ovaries and has spread to other organs in the pelvis, or there is primary peritoneal cancer. It has not spread to nearby lymph nodes or to distant sites.
AJCC and FIGO Stage IIA:
- The cancer has spread or invaded the uterus or fallopian tubes. It has not spread to nearby lymph nodes or to distant sites.
AJCC and FIGO Stage IIB:
- The cancer is on the outer surface of or has grown into other nearby pelvic organs, such as the bladder, the sigmoid colon, or the rectum. It has not spread to nearby lymph nodes or to distant sites.
AJCC and FIGO Stage IIIA1:
- The cancer is in one or both ovaries, or there is primary peritoneal cancer, and it may have spread to nearby pelvic organs. It has spread to the retroperitoneal lymph nodes but not to distant sites.
AJCC and FIGO Stage IIIA2:
- The cancer is in one or both ovaries, or there is primary peritoneal cancer, and it has spread or grown into other organs outside the pelvis. During surgery, no cancer can be seen in the belly, but tiny deposits of cancer are found in the lining of the abdomen when it is looked at in the lab. The cancer may or may not have spread to retroperitoneal lymph nodes, but not to distant sites.
AJCC and FIGO Stage IIIB:
- There is cancer in one or both ovaries, or there is primary peritoneal cancer, and it has spread to organs outside the pelvis. The surgeon can see the cancer, but it is no bigger than 2cm across. It may or may not have spread to the retroperitoneal lymph nodes, but has not spread to the inside of the liver or spleen or distant sites.
AJCC and FIGO Stage IIIC:
- The cancer is in one or both of the ovaries, and there is primary peritoneal cancer, and it has spread to organs outside the pelvis. The cancer is larger than 2 cm across and may be on the outside of the liver or spleen. It may or may not spread to the retroperitoneal lymph nodes, but has not spread to the inside of the liver or spleen or distant sites.
AJCC and FIGO Stage IVA:
- Cancer cells are found in the fluid around the lungs with no other cancer spread.
AJCC and FIGO Stage IVB:
- The cancer has spread to the inside of the spleen or liver, lymph nodes that are not in the retroperitoneal area, and/or to organs or tissues outside the peritoneal cavity.
How is ovarian cancer treated?
Treatment for ovarian cancer depends on many factors, like your cancer stage, age, overall health, and testing results. Your treatment may include:
- Surgery.
- Radiation Therapy.
- Chemotherapy.
- Hormone Therapy.
- Targeted Therapy.
- Immunotherapy.
- Clinical Trials.
Surgery
Surgery is the most common treatment for ovarian cancer. If you have surgery to stage your cancer, it is likely that your surgeon will also “debulk” your tumor during this surgery. “Debulking” means your surgeon will remove as much of the tumor as possible.
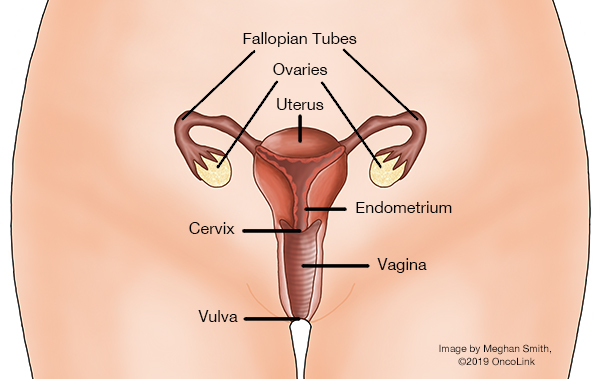
Surgery to stage ovarian cancer often removes your uterus (called a “hysterectomy”) and your fallopian tubes and ovaries (called a “bilateral salpingo-oophorectomy” or BSO). The layer of fat that covers the muscles in your abdomen (belly) is also removed. Some nearby lymph nodes may also be removed to test for cancer.
Surgery to debulk ovarian cancer depends on where the cancer has spread (metastasized). During debulking surgery, other organs may need to be removed. These include part or all of your:
- Colon.
- Bladder.
- Spleen.
- Gallbladder.
- Liver.
- Pancreas.
- Stomach.
To read more about surgeries used for ovarian cancer, see our article “Surgical Procedures: Surgical Staging for Ovarian (Epithelial), Primary Peritoneal and Fallopian Tube Cancer.”
Radiation Therapy
Radiation is the use of high-energy x-rays to kill cancer cells. Radiation is useful in treating areas where the cancer may have spread.
Two types of radiation therapy are used for ovarian cancer:
- External beam radiation therapy (EBRT): The radiation is delivered from the outside of your body and focused on your ovaries and nearby areas.
- Brachytherapy (internal radiation therapy): A radioactive source is placed inside your vagina.
Chemotherapy
Chemotherapy is the use of anti-cancer medications to treat cancer. In most cases, more than one chemotherapy medication will be used for your treatment. Some chemotherapy medications you may receive are cisplatin, carboplatin, paclitaxel, docetaxel, nab-paclitaxel, altretamine, capecitabine, cyclophosphamide, etoposide, gemcitabine, ifosfamide, irinotecanliposomal doxorubicin, melphalan, pemetrexed, topotecan, vinorelbine, bleomycin, vinblastine, and dactinomycin.
Hormone Therapy
Some cancers need hormones to grow. Blocking the action of these hormones might stop the cancer from growing. Some hormone therapy medications used to treat ovarian cancer are goserelin, leuprolide, tamoxifen, letrozole, anastrozole, and exemestane
Targeted Therapy
Targeted therapies are medications that target something specific to the cancer cells, stopping them from growing and dividing. Some types of targeted therapy used for ovarian cancer are olaparib, rucaparib, niraparib, bevacizumab, mirvetuximabsoravtansine, larotrectinib,dabrafenib, trametinib, fam-trastuzumab deruxtecan-nxki, selpercatinib, and entrectinib.
Immunotherapy
Immunotherapy is the use of medication to help your immune system fight cancer. Immunotherapy medications used to treat ovarian cancer include dostrarlimab-gxly and pembrolizumab. This medication is an immune checkpoint inhibitor that blockd a protein called PD-1. By blocking PD-1, this medication helps your immune system decrease tumor size or slow down cancer cell division.
Clinical Trials
You may be offered a clinical trial as part of your treatment plan. To find out more about current clinical trials, visit the OncoLink Clinical Trials Matching Service.
Making Treatment Decisions
Your care team will include you when choosing your treatment plan. This can be overwhelming as you may be given a few options to choose from. It can take a few weeks to meet with different providers and think about your options and what is best for you. This is a personal decision. Friends and family can help you talk through the options and the pros and cons of each, but they cannot decide for you. You need to be comfortable with your decision – this will help you move on to the next steps. If you ever have any questions or concerns, be sure to call your team.
You can learn more about ovarian cancer at OncoLink.org.