Surgical Procedures: Pneumonectomy
What is a pneumonectomy and how is it done?
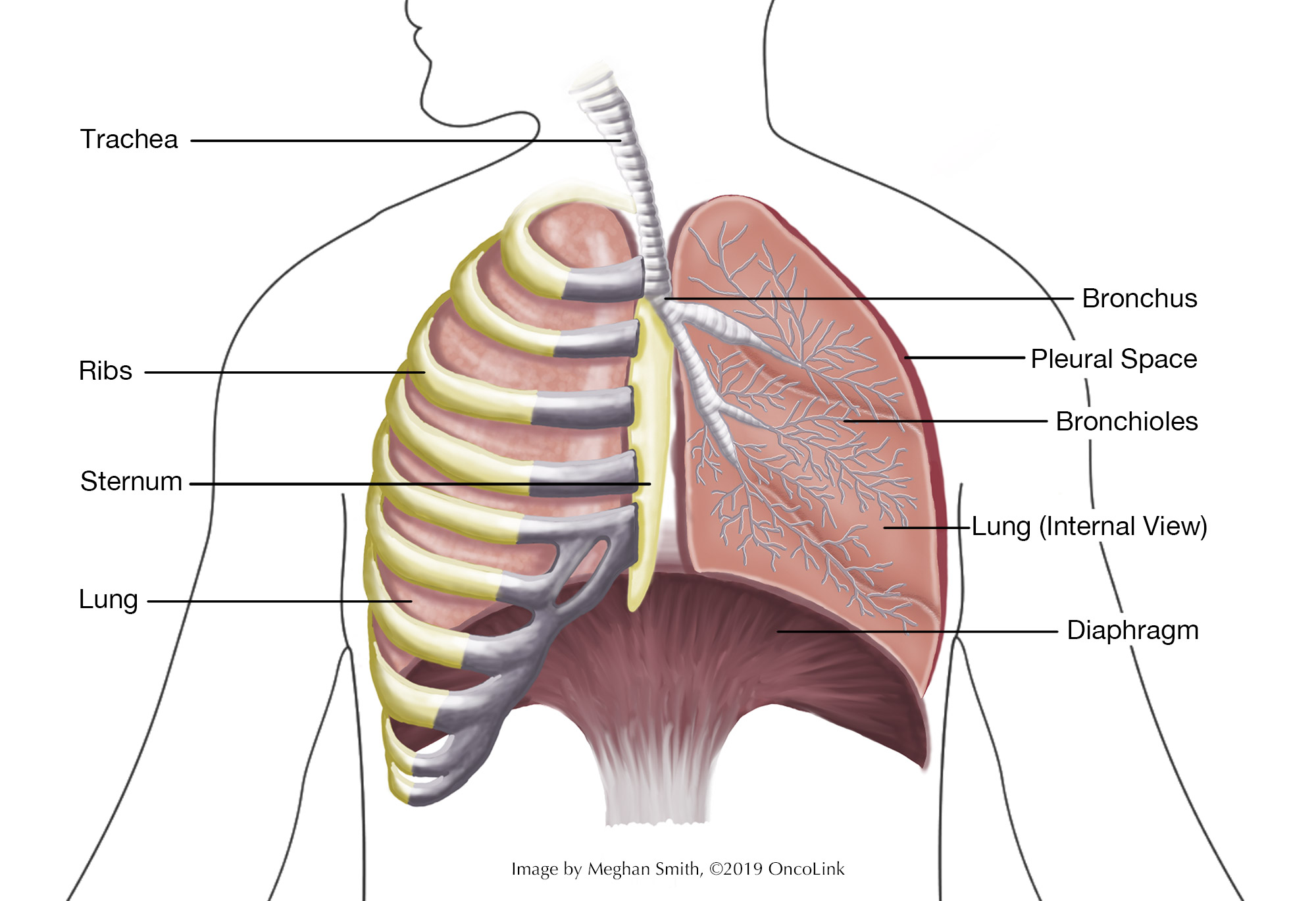
A pneumonectomy is the removal of a lung. The lungs are two large organs in each side of your chest cavity. Your lungs filter oxygen and put it into your blood. Lungs also keep us safe from harmful things in the air that we may breathe in. The lungs make mucus, which traps things like smoke, pollution, bacteria, and viruses. This mucus is then removed from the body by coughing and/or swallowing.
Each lung is made up of lobes or sections. The left lung has two lobes. The right has three lobes and is larger.
A pneumonectomy may be used to treat:
- Lung cancer.
- Malignant mesothelioma.
- Traumatic injury.
- Disseminated thymomas.
- Bronchial obstruction.
- Congenital lung disease.
- Lung infections, such as tuberculosis (TB).
There are two types of pneumonectomies:
- Traditional/Standard Pneumonectomy:The whole lung is removed.
- Extrapleural Pneumonectomy:The whole lung is removed, as well as a part of the membrane that covers the heart (pericardium), part of the diaphragm (a muscle that helps us breathe in and out), and the membrane that lines the inside of the chest (pleura).
A pneumonectomy is done during a surgery called a thoracotomy. During a thoracotomy, an incision (cut) is made between two ribs, from the front of the chest around to the back. This lets the surgeon remove the lung and anything else that needs to be removed.
What are the risks of a pneumonectomy?
There are risks and side effects related to a pneumonectomy. Risks and side effects may be:
- Need for a machine to help you breathe (ventilator/respirator).
- Reaction to anesthesia (Anesthesia is the medication you are given to help you sleep through the surgery, to not remember it, and to manage pain. Reactions can include wheezing, rash, swelling, and low blood pressure).
- Bleeding.
- Heart issues, such as arrhythmias (irregular heartbeat) and heart attack.
- Pulmonary embolism (blood clot in the lung).
- Pneumonia.
- Infection at the incision (surgical cut) site.
- Broncopleural fistula (an abnormal connection between the bronchus and pleural space).
- Pleural abscess called an empyema, and/or fluid in the lungs.
- Organ failure, such as kidney failure.
- Injury to nearby lung and/or blood vessels.
- Long term shortness of breath and/or the need for long term oxygen.
- Postpneumonectomy syndrome (When other organs in the chest fill the empty cavity where the lung was removed. A prosthesis (an artificial body part) may be needed to fill the space).
Your surgeon and healthcare team will talk with you about the risks of your procedure.
What is recovery like?
Recovery from a pneumonectomy depends on the procedure you had. Often, a 7-10 day hospital stay is needed. After surgery, you will be on a ventilator/respirator and have tubes in your chest that will remove extra fluid and/or air.
You will be told how to care for your incisions and will be given any other instructions before leaving the hospital.
Your medical team will teach you about the medications you will be taking for pain, blood clot, infection, and constipation prevention, and/or other conditions.
Your provider will talk to you about how to care for yourself and any changes in activity you will need to make. In general:
- Keep your incisions clean and dry. Don’t use creams, lotions, or ointments unless told to do so.
- Rest. Feeling tired and fatigued is a normal part of recovery.
- Do not do activities that cause pain.
- Do not lift anything heavy.
- When lying down, lie on the side where you had surgery so your remaining lung is facing upward.
- Avoid smoking and second-hand smoke. If you would like help quitting, speak to your provider.
- You can often return to work around 8 weeks after surgery, depending on the type of job you have and if you have fully recovered.
- Do not drive while taking narcotic pain medication.
- Take and record your pulse (heart rate) as directed.
- Be sure to use your incentive spirometer and cough as directed by your healthcare team. You may need to use it 5-10 times per day for 2 weeks.
- Use supplemental oxygen as directed by your healthcare team.
What will I need at home?
- Thermometer to check for fever, which can be a sign of infection. Your care team will tell you at what temperature you should call them.
- Write down your vital signs and any changes you notice.
- Wound care and oxygen supplies, which are given to you by the hospital or your provider’s office.
When should I call my healthcare team?
- If you have a fever. Your care team will tell you at what temperature they should be called.
- Drainage, redness, swelling, or pain at your incision.
- Nausea or vomiting.
- New or worse pain.
- Shortness of breath, chest pain, or bloody, yellow, green, or brown sputum (mucus you cough up).
- Swelling in one or both legs.
- Irregular, racing, or abnormal heartbeat.
Seek medical attention RIGHT AWAY if:
- You are having chest pain or a hard time breathing.
- Your surgical bandage is soaking with blood.
- Your incision comes apart (separates).
- You are coughing up blood (more than a teaspoon) or you have a lot of brown/bloody sputum.
- If you are in distress, call 911 and lie on the side that you had the surgery on, leaving your remaining lung facing upward.
How can I care for myself?
You may need a family member or friend to help you with your daily tasks until you are feeling better. It may take some time before your team tells you that it is ok to go back to your normal activity.
Be sure to take your prescribed medications as directed to prevent pain, infection, and/or constipation. Call your team with any new or worsening symptoms.
There are ways to manage constipation after your surgery. You can change your diet, drink more fluids, and take over-the-counter medications. Talk with your care team before taking any medications for constipation.
Taking deep breaths and resting can help manage pain, keep your lungs healthy after anesthesia, and promote good drainage of lymphatic fluid. Try to do deep breathing and relaxation exercises a few times a day in the first week, or when you notice you are extra tense.
- Example of a relaxation exercise: While sitting, close your eyes and take 5-10 slow deep breaths. Relax your muscles. Slowly roll your head and shoulders.
This article contains general information. Please be sure to talk to your care team about your specific plan and recovery.