Surgical Procedures: Surgical Staging for Cervical Cancer
What is cervical cancer?
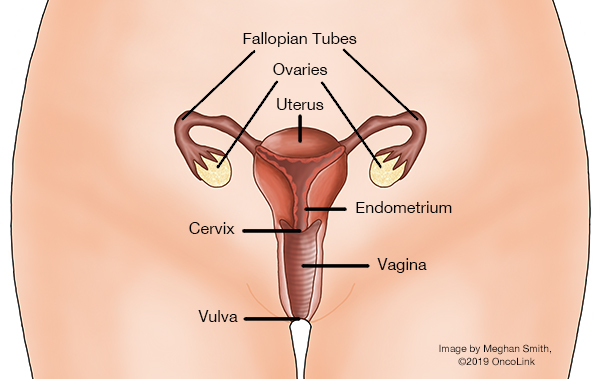
When there are cancer cells in the tissue of the uterine cervix, it is called cervical cancer. Cervical cancer is often caused by the human papillomavirus (HPV).
What is staging and how is it done?
Staging is a way to find out how far the cancer has spread in your body. Your provider will have you get a few tests to figure out the stage of your cancer. For cervical cancer, these tests may be:
- CT scan.
- Positron emission tomography scan (PET scan).
- Magnetic resonance imaging (MRI).
- Ultrasound.
- Chest X-Ray.
- IVP (intravenous pyelogram, which looks at urinary structures).
In some cases, you may have a cystoscopy (to look inside your bladder) or a proctoscopy (to look inside your rectum). Surgery may be used to stage the cancer before any other treatment.
Cervical cancer can spread to other parts of your body through the lymph and blood systems. Once your provider knows your stage of cancer, they can help plan your treatment.
Two staging systems are used to figure out the stage of your cancer:
- The FIGO staging system (International Federation of Gynecology and Obstetrics).
- The American Joint Committee on Cancer TNM staging system.
Both of these staging systems will give your healthcare team information on the extent of the tumor (T), spread to the lymph nodes (N) and distant metastasis (spread) (M).
What surgical procedures are used to diagnose and treat cervical cancer?
It is often recommended that if you have stage 0 (carcinoma in-situ) to stage IVA (4A) cervical cancer, you have surgery. There are many surgeries that may be used, based on your stage and situation. They include:
- Cervical Conization: Removal of a cone-shaped wedge from your cervix and cervical canal. This can be used to diagnose and/or treat the cancer. This may be done using:
- Cold-Knife Cone (CKC): A scalpel is used to remove the area.
- Loop Electrosurgical Excision Procedure (LEEP): A wire with an electrical current is used.
- Laser: A laser beam is used to remove precancerous lesions on the surface of your cervix.
- Cryosurgery: Liquid nitrogen is applied to pre-cancerous cells in your vagina and cervix.
- Total Hysterectomy: Your uterus and cervix are removed. In some cases, your ovaries and fallopian tubes will not be removed and will be kept in place.
- Radical Hysterectomy: Your uterus, cervix, tissue around the cervix, and the upper part of your vagina are removed. Your fallopian tubes and lymph nodes may or may not be removed.
- Modified Radical Hysterectomy: Your uterus, cervix, tissue/ligaments around your cervix, and the upper part of your vagina are removed. Some lymph nodes may or may not be removed.
- Radical Trachelectomy: Your cervix, nearby tissue, lymph nodes and upper vagina are removed, leaving behind the uterus and ovaries.
- Bilateral Salpingo-Oophorectomy (BSO): Your ovaries and fallopian tubes on both sides are removed.
- Pelvic Exenteration: Your uterus, cervix, ovaries, fallopian tubes, vagina are removed. At times, your bladder, urethra and/or bowel, anus and rectum are also removed.
- Pelvic Lymph Node Dissection: Your lymph nodes are removed to test for metastatic cancer (cancer that has spread).
A hysterectomy can be done a few ways, such as:
- Abdominal (Belly): An incision is made into your abdomen (belly) to remove the uterus.
- Vaginal: An incision is made in your upper vagina, and your uterus is removed through this cut.
- Laparoscopic: A laparoscope (lighted tube with a camera) is used. Certain tools are used to make small incisions in your abdomen.
- Robotic: The surgeon controls a robotic arm to perform the surgery through small incisions.
What is recovery like?
Recovery from surgery for cervical cancer will include a stay in the hospital for one to several days, depending on the type of procedure you had.
When you are home, take your prescribed medications as you are told to prevent pain, infection and/or constipation. Call your team with any new or worsening symptoms.
Your healthcare provider will talk with you about any changes you will need to make to your daily activities.
How can I care for myself?
You may need a family member or friend to help you with your daily tasks until you are feeling better. It may take some time before your team tells you that it is ok to go back to your normal activity.
Be sure to take your prescribed medications as directed to prevent pain, infection and/or constipation. Call your team with any new or worsening symptoms.
There are ways to manage constipation after your surgery. You can change your diet, drink more fluids, and take over-the-counter medications. Talk with your care team before taking any medications for constipation.
Taking deep breaths and resting can help manage pain, keep your lungs healthy after anesthesia, and promote good drainage of lymphatic fluid. Try to do deep breathing and relaxation exercises a few times a day in the first week, or when you notice you are extra tense.
- Example of a relaxation exercise: While sitting, close your eyes and take 5-10 slow deep breaths. Relax your muscles. Slowly roll your head and shoulders.
This article contains general information. Please be sure to talk to your care team about your specific plan and recovery.