Sentinel Lymph Node Biopsy: The Basics
What is the lymph system?
The lymph system is the "housekeeping system" of the body. The lymph system:
- Is a network of vessels (tubes) that connects hundreds of lymph nodes all over your body. These nodes are about 2 centimeters (cm) in size.
- Lymph nodes have cells that help clear out bacteria and other things that shouldn’t be in your body.
- Lymph is fluid that flows between cells in your body. This fluid picks up things like bacteria and takes them into a lymph node for filtering. The bacteria or other things pass through more nodes in the system before going into your bloodstream and then are cleared by your liver.
- Your spleen and thymus gland are also part of your lymph system.
- Cancer cells can spread to other parts of your body through the lymph system. Because of this, lymph nodes are one of the earliest sites of spread (metastasis) for some cancers.
A sentinel lymph node(s) is the lymph node(s) where cancer cells spread first from the primary (original) tumor.
What is a sentinel lymph node biopsy?
A sentinel lymph node biopsy (SLB), also called an SLN biopsy, is a surgery to see if there are cancer cells in the sentinel lymph node. During an SLB, the surgeon finds the sentinel lymph node(s), removes it, and tests it to see if cancer cells are in the node. This biopsy is often done during surgery to remove the primary tumor. An SLB can also be done on its own, either before or after your primary tumor is removed.
How is a sentinel lymph node biopsy done?
A sentinel lymph node biopsy can be done in an outpatient setting or in the hospital. In some cases, you will stay overnight in the hospital. You will be given medication that will help you sleep and not remember the surgery (general anesthesia) so you will need a ride home if you are sent home after the biopsy.
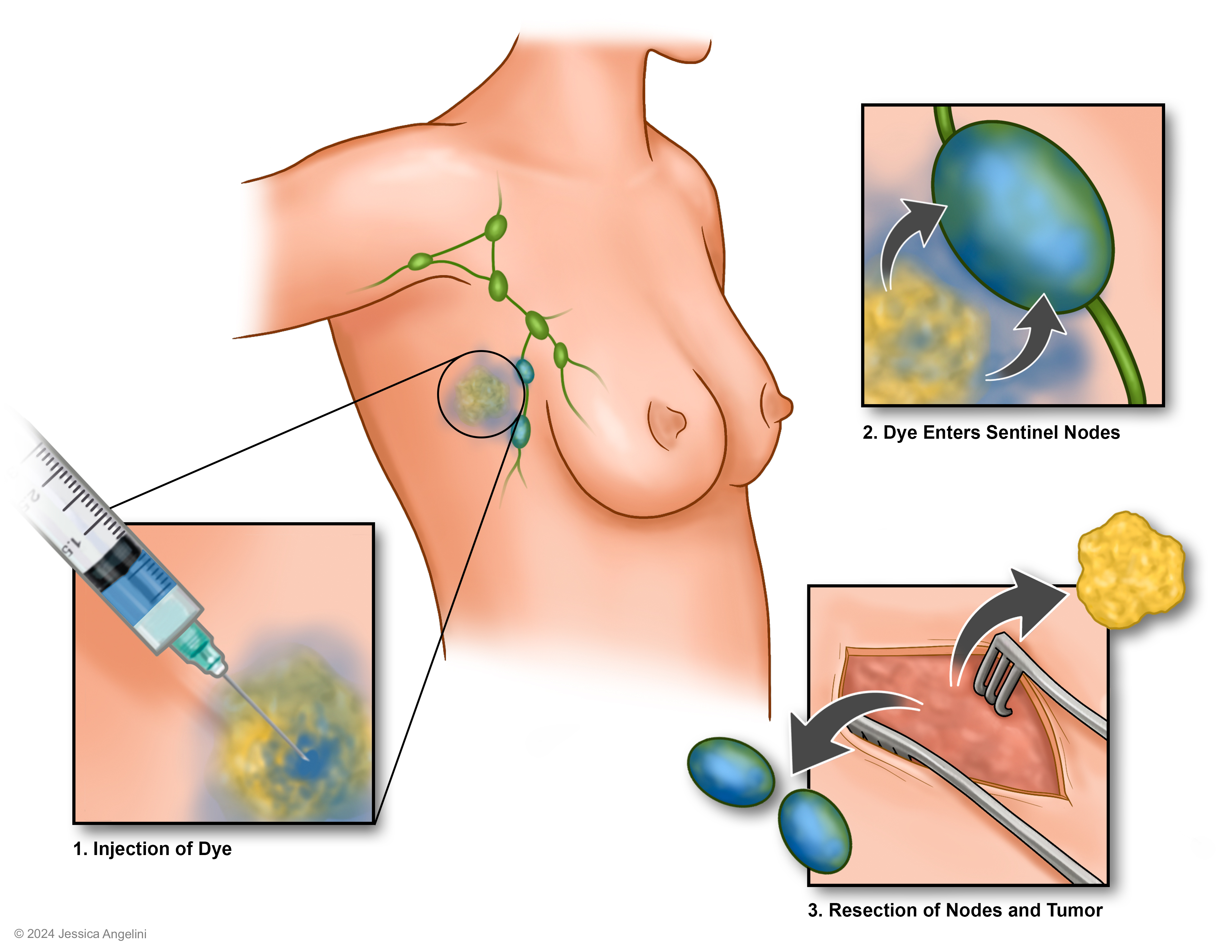
- You will have either a blue dye or a radioactive material (in some cases both) injected (put in) near the tumor or in the area where the tumor was removed. This is done either in the nuclear medicine department or in the operating room (OR) a few hours before the biopsy.
- The dye/radioactive material goes through your lymph system to the sentinel node(s). The surgeon uses a tool that looks for the dye to find the sentinel lymph node. The surgeon can see which lymph node(s) it goes to first (the sentinel node).
- Once the sentinel lymph node is removed, a pathologist will check for cancer cells under a microscope.
- If cancer cells are found, the surgeon may want to go back and remove more lymph nodes.
- The incision (surgical cut) is closed with sutures (stitches) or glue, and it will be covered by a bandage.
Why is only the sentinel lymph node(s) removed?
Removing only the sentinel lymph node(s) lets your surgeon leave your other lymph nodes intact. When more lymph nodes are removed, there is a risk of lymphedema. Lymphedema happens when the lymph fluid cannot drain from the area (most often an arm, leg, or the head/neck). This leads to swelling that can be painful. Lymphedema can make it hard to use or move that limb and puts you at higher risk of serious infection in that limb.
What are the risks of a sentinel lymph node biopsy?
A sentinel lymph node biopsy has some risks and possible side effects. These risks may be:
- Pain and/or bruising at the incision site.
- A small pocket of fluid under the incision (called a seroma).
- Swelling.
- Infection.
- An allergic reaction to the blue dye used.
- The risk of lymphedema is much lower with SLB, but it is not zero. If you have any swelling in the arm or leg where the SLB was done, tell your provider right away.
A sentinel lymph node biopsy can help stage your cancer and avoid more extensive surgery. The more lymph nodes that are removed, the greater the risk of other, more serious side effects, like lymphedema, seroma, numbness and tingling at the surgical site, and being unable to move the affected body part. To learn more about the procedure and what to expect, read Surgical Procedures: Sentinel Lymph Node Biopsy.