Proton Radiation Therapy Treatment Process
If proton radiation therapy might be part of your treatment plan, you will have an initial consultation where you talk to a radiation oncologist. If you decide to have this treatment, you will sign a consent form and will need to be set up for treatment. Getting set up for radiation takes many steps, many providers, and can take a few days or weeks. The steps may change a little based on your treatment facility. If your treatment is being done urgently, the order and timing of these steps may be different.
CT Simulation
Before your radiation treatments begin, you will go through a treatment planning process called "simulation." During this process, your radiation treatment team will measure your body and mark on your skin where you will get radiation. The marks will be made with a temporary paint marker and/or a small set of permanent tattoos. The position you are in for your simulation will be the same position you will be in every day for treatment. Immobilization devices such as molds, casts, headrests, knee supports, or other devices may be used to help keep you in a comfortable position and make sure you don’t move during treatment.
A CT scan of the area being treated is done. The images from the CT scan are used to make your treatment plan and create a "map" for the treatment team. This CT scan is used only for the planning process, it is not a replacement for other imaging scans you have had or may need. During your simulation, you may need contrast which is a dye that will make certain parts of your body more visible in the CT images. This can be given by drinking it (orally) or putting (injecting) it directly into your vein (intravenously).
You may be given directions if any preparation (prep) is needed before your simulation. For example, your bowels may need to be empty so you may have to take certain medications, do an enema, or eat a certain diet. You need to follow the directions closely. If you have any questions or are having trouble with the prep you should call your provider.
The simulation takes about an hour. You will be lying on a hard table for the simulation, and you may have some pain or discomfort. Tell the radiation therapists if you are uncomfortable right away so they can change your position. Keep in mind that the time needed to deliver the radiation therapy treatments is often much less than the time needed for the simulation.
In certain cases, an MRI or a PET scan will also be done the same day as the CT simulation. The images from these scans are also used to plan your treatment.
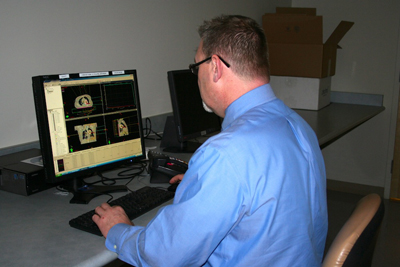
Technical Planning Process
After simulation, details are looked at by the medical dosimetrists and physicists (members of your radiation team). They figure out the exact dose and course of treatment with the goal of killing the cancer while limiting damage to healthy tissue. They use proton treatment planning software to help them design the best possible treatment plan. The dosimetrist and physicist work closely with your radiation oncologist to create your treatment plan. This can take up to a week or more.
Quality Assurance
After the radiation oncologist approves your treatment plan the physicists will check that your specific plan works on the proton machine it was created for. Once this is done you can start your radiation treatments.
Set-Up
You will need to be on the treatment table in the same position you were in for your simulation. The therapists will line up your tattoos with the lasers in the treatment room and take a set of X-ray films or do a cone-beam computed tomography (CBCT). CBCT is an imaging technique that makes a 3D representation of the body and tumor from a rotating scan. These films will be matched with the simulation films to make sure the treatment is given to the right area. You may be asked to move your body to get in the right position for treatment. Your oncologist will check your films before the radiation is given. This is standard practice to ensure the most accurate beam delivery. Once your films and position are confirmed the setup is done and the radiation can be given.
Your set-up appointment may be scheduled the day before you start radiation, or it may be scheduled along with your first day of radiation. This is based on the preference or availability of the facility where you are being treated.
Daily Treatments
Treatments are often given once a day, Monday through Friday, for a number of weeks. Sometimes, twice daily radiation treatments will be given. It takes about 5 minutes to get your radiation treatment, but you will likely be scheduled for 25-30 minutes in the treatment room. With set up and treatment your total appointment time will be about one hour each day. This allows time for you to get changed, do any preparation, be positioned on the treatment table, get your treatment, and for the therapists to clean all the equipment and setup the room of the next patient. Some things that may affect the total time of your treatment include:
- The number of treatment fields.
- The type of imaging being used for your setup.
- How long it takes to position you for treatment.
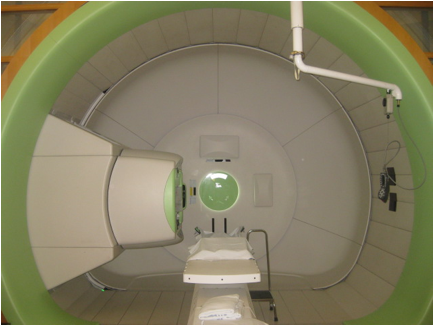
Each day, the therapists will help position you on the treatment table, using the tattoos, immobilization devices, and laser beams on the machine to get you in the exact same position. The therapists will leave the room while giving the radiation to avoid exposure. They will be able to see and hear you from a control room just outside the treatment room. They can also give you instructions over a microphone during the treatment. As you lie on the treatment table, the table and gantry (part of the radiation machine) may move to get the proton beams in the right location. The treatment is not painful, and you will not feel anything during treatment.
Imaging is done daily prior to treatment to make sure you are in the best position possible for treatment. More imaging may be done weekly to see if your plan needs to change. If changes are needed, imaging will be done on the first day of the new plan. The images taken during your radiation treatments are not used to see if your cancer is responding to the radiation. They are used to make sure that the position and arrangement for treatment are correct.
In some cases, when aligning you for treatment, your position may not be the best. In these cases, the radiation therapists will talk with your oncologist about what to do. Sometimes the treatment plan needs to be adjusted and treatment may need to be paused until a new plan is created. If this happens you will need a new simulation.
On-Treatment Visit
Your radiation oncologist will meet with you at least once a week.
The visit will take place just before or after your treatment is given. These visits give your provider a chance to see how you are doing, answer any questions you have, and plan future treatments.
If you are having a problem, you do not have to wait until your next visit. Instead, you can call your radiation team’s office and ask to be seen or to talk to a medical provider. A provider will review your problem or concern and if they cannot help, they will contact your oncologist. If you have any problems at night or on the weekends, call the hospital operator and ask for "the radiation oncologist-on-call."
End-Of-Treatment Visit
A day or two before your last treatment, you will have your final on-treatment visit with your provider. During this visit, they will talk to you about follow-up care and may do an exam.
Follow-Up Care
Follow-up appointments are often scheduled at 4 and 12 weeks after your radiation treatments are done. You may be asked to have a scan (CT, PET, or MRI) before this visit. Your provider will see how you are doing and talk to you about further follow-up care. It is important to go to your follow-up care appointments so that any radiation-related problems can be found and treated early. Your radiation providers will also continue to consult with your other cancer specialists.
Resources for More Information
Preparing for Radiation: Simulation and Treatment
References
Cancer.Net. What is Radiation Therapy? 2022.
Cancer.Net. What to Expect When Having Radiation Therapy. 2022.
Mayo Clinic. Radiation Therapy. 2023.
National Cancer Institute. Radiation Therapy to Treat Cancer. 2019.
Stony Brook Cancer Center. Radiation Therapy Process. 2022.