Vaginal Cancer: Staging and Treatment
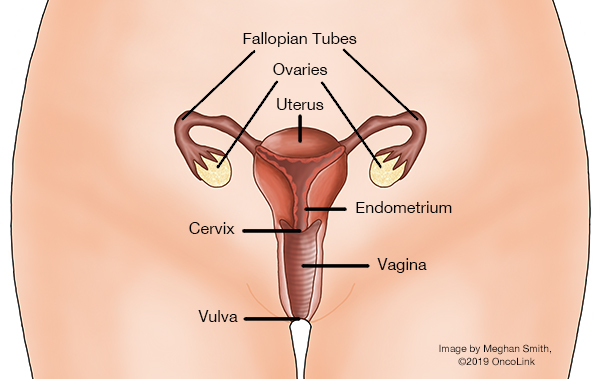
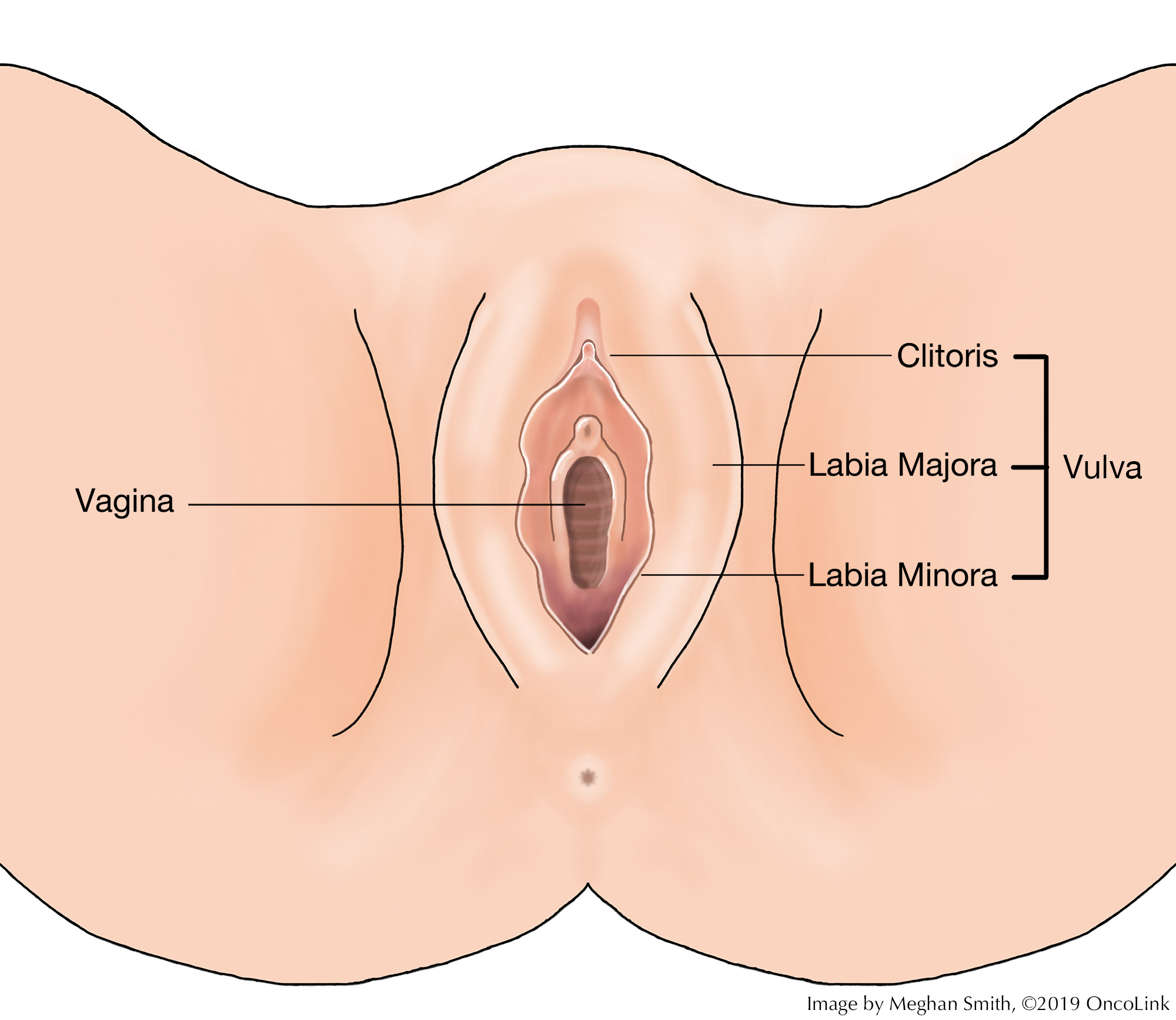
What is the vagina?
The vagina, also called the "birth canal," is a 3 to 4-inch hollow tube that runs from the vulva (outside genitalia) up to the cervix (the lower part of the uterus/womb). The walls of the vagina are often in a "closed" or collapsed position but can widen during sex or the delivery of a baby.
What is staging for cancer?
Staging is the process of learning how much cancer is in your body and where it is. Tests like a pelvic exam, Pap test, biopsy, CT, and MRI are done to help stage your cancer. Your providers need to know about your cancer and your health so that they can plan the best treatment for you.
Staging looks at the size of the tumor, where it is, and if it has spread to other organs. The two staging systems for vaginal cancer are the FIGO (International Federation of Gynecology and Obstetrics) system and the TNM system from the American Joint Committee on Cancer. They each have 3 parts used to stage vaginal cancer:
- T-Describes the size/location/extent of the cancer.
- N-Describes if the cancer has spread to the lymph nodes.
- M-Describes if the cancer has spread to other organs (metastases).
Your healthcare provider will use the results of the tests you had to determine your stage.
How is vaginal cancer staged?
Vaginal cancer is often staged before you have surgery, called clinical staging. It is based on the results of:
- Your physical exam.
- Imaging Tests.
- Biopsies.
Staging is important because it helps guide your treatment options.
The staging system is very complex. Below is a summary of the staging system. Talk to your provider about the stage of your cancer.
AJCC Stage IA; Stage Grouping T1am N0, M0; FIGO Stage I: The cancer is only in the vagina and is no more than 2cm (centimeters). It has not spread to the lymph nodes or other organs.
AJCC Stage IB; Stage Grouping T1b, N0, M0; FIGO Stage I: The cancer is only in the vagina and is larger than 2cm. It has not spread to lymph nodes or other organs.
AJCC Stage IB; Stage Grouping T1b, N0, M0; FIGO Stage I: The cancer is only in the vaginal wall and is bigger than 2cm. It has not spread to the lymph nodes or other parts of the body.
AJCC Stage IIA; Stage Grouping T2a, N0, M0; FIGO Stage II: The cancer has grown through the vaginal wall but not into the pelvic wall. It is no larger than 2cm and has not spread to the lymph nodes or other parts of the body.
AJCC Stage IIB; Stage Grouping T2b, N0, M0; FIGO Stage II: The cancer has grown through the vaginal wall but not into the pelvic wall. It is bigger than 2cm and has not spread to the lymph nodes or other organs.
AJCC Stage III; Stage Grouping T1 to T3, N1, M0; FIGO Stage III: The cancer is any size, may be growing into the pelvic wall and/or has blocked urine flow (causes the kidneys to not work). It has spread to lymph nodes but not to other parts of the body.
AJCC Stage III; Stage Grouping T3, N0, M0; FIGO Stage III: The cancer is growing into the pelvic wall and/or has blocked the flow of urine causing kidney damage. It has not spread to lymph nodes or other parts of the body.
AJCC Stage IVA; Stage Grouping T4, Any N, M0; FIGO Stage IVA: The cancer is growing into the bladder or rectum or out of the pelvis. It may or may not have spread to lymph nodes in the pelvis or groin and has not spread to other parts of the body.
AJCC Stage IVB; Stage Grouping Any T, Any N, M1; FIGO Stage IVB: The cancer has spread to other parts of the body like the lungs, liver, or bones. It is any size and may or may not have grown into nearby structures and lymph nodes.
How is vaginal cancer treated?
Treatment for vaginal cancer depends on things like your cancer stage, age, overall health, and testing results. There is no “standard” treatment for vaginal cancer and each person’s treatment plan will be different. Your treatment may include:
Surgery
If you have a small lesion(s) in the upper vagina, you may have surgery. This surgery will remove all or part of the vagina (vaginectomy). You may need reconstructive surgery after a vaginectomy. This is when the surgeon makes a vaginal canal using a skin or muscle flap taken from another part of the body. You may also need a hysterectomy.
Chemotherapy may be given before surgery to help shrink the tumor (called neoadjuvant chemotherapy).
Chemotherapy
Chemotherapy is the use of medications to kill cancer cells throughout the body. One treatment option is a cisplatin-based chemotherapy used with radiation. Other chemotherapies used are carboplatin, fluorouracil, paclitaxel, and docetaxel. Chemotherapy can also be used to control recurrent (cancer that comes back) or widespread cancer.
Radiation
Radiation therapy uses high-energy x-rays to kill cancer cells. It can be used to treat invasive vaginal cancer. It can be treated using external beam radiation, brachytherapy (internal radiation), or a combination of both. If cancer returns after treatment with radiation, surgery is often needed.
Clinical Trials
You may be offered a clinical trial as part of your treatment plan. To find out more about current clinical trials, visit the OncoLink Clinical Trials Matching Service.
Making Treatment Decisions
Your care team will make sure you are included in choosing your treatment plan. This can be overwhelming as you may be given a few options to choose from. It feels like an emergency, but you can take a few weeks to meet with different providers and think about your options and what is best for you. This is a personal decision. Friends and family can help you talk through the options and the pros and cons of each, but they cannot make the decision for you. You need to be comfortable with your decision – this will help you move on to the next steps. If you ever have any questions or concerns, be sure to call your team.
You can learn more about vaginal cancer at OncoLink.org.